
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Metabolic Risk/Epidemiology
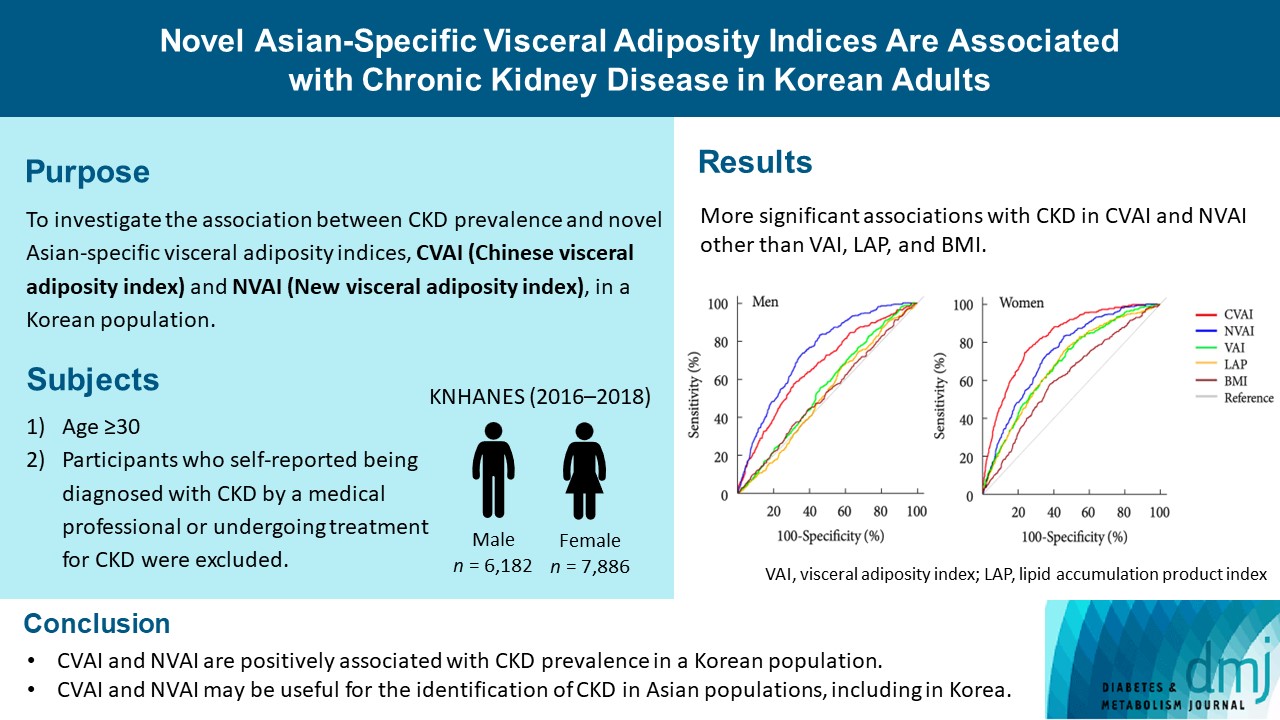
- Novel Asian-Specific Visceral Adiposity Indices Are Associated with Chronic Kidney Disease in Korean Adults
- Jonghwa Jin, Hyein Woo, Youngeun Jang, Won-Ki Lee, Jung-Guk Kim, In-Kyu Lee, Keun-Gyu Park, Yeon-Kyung Choi
- Diabetes Metab J. 2023;47(3):426-436. Published online March 6, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0099
- 2,478 View
- 128 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The Chinese visceral adiposity index (CVAI) and new visceral adiposity index (NVAI) are novel indices of visceral adiposity used to predict metabolic and cardiovascular diseases in Asian populations. However, the relationships of CVAI and NVAI with chronic kidney disease (CKD) have not been investigated. We aimed to characterize the relationships of CVAI and NVAI with the prevalence of CKD in Korean adults.
Methods
A total of 14,068 participants in the 7th Korea National Health and Nutrition Examination Survey (6,182 men and 7,886 women) were included. Receiver operating characteristic (ROC) analyses were employed to compare the associations between indices of adiposity and CKD, and a logistic regression model was used to characterize the relationships of CVAI and NVAI with CKD prevalence.
Results
The areas under the ROC curves for CVAI and NVAI were significantly larger than for the other indices, including the visceral adiposity index and lipid accumulation product, in both men and women (all P<0.001). In addition, high CVAI or NVAI was significantly associated with a high CKD prevalence in both men (odds ratio [OR], 2.14; 95% confidence interval [CI], 1.31 to 3.48 in CVAI and OR, 6.47; 95% CI, 2.91 to 14.38 in NVAI, P<0.05) and women (OR, 4.87; 95% CI, 1.85 to 12.79 in CVAI and OR, 3.03; 95% CI, 1.35 to 6.82 in NVAI, P<0.05); this association remained significant after adjustment for multiple confounding factors in men and women.
Conclusion
CVAI and NVAI are positively associated with CKD prevalence in a Korean population. CVAI and NVAI may be useful for the identification of CKD in Asian populations, including in Korea. -
Citations
Citations to this article as recorded by- Association between Chinese visceral adiposity index and risk of stroke incidence in middle-aged and elderly Chinese population: evidence from a large national cohort study
Zenglei Zhang, Lin Zhao, Yiting Lu, Xu Meng, Xianliang Zhou
Journal of Translational Medicine.2023;[Epub] CrossRef
- Association between Chinese visceral adiposity index and risk of stroke incidence in middle-aged and elderly Chinese population: evidence from a large national cohort study
- Impact of Social Distancing Due to Coronavirus Disease 2019 on the Changes in Glycosylated Hemoglobin Level in People with Type 2 Diabetes Mellitus (Diabetes Metab J 2021;45:109-14)
- Sung-Don Park, Sung-Woo Kim, Jun Sung Moon, Jae-Han Jeon, Mi Kyung Kim, Keun-Gyu Park
- Diabetes Metab J. 2021;45(2):279-280. Published online March 25, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0300
- 4,212 View
- 87 Download
- 1 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- A cross-sectional study on the telemedicine usage and glycemic status of diabetic patients during the COVID-19 pandemic
Novi Sulistia Wati, Pokkate Wongsasuluk, Pradana Soewondo
Medical Journal of Indonesia.2021; 30(3): 215. CrossRef
- A cross-sectional study on the telemedicine usage and glycemic status of diabetic patients during the COVID-19 pandemic
- COVID-19
- Impact of Social Distancing Due to Coronavirus Disease 2019 on the Changes in Glycosylated Hemoglobin Level in People with Type 2 Diabetes Mellitus
- Sung-Don Park, Sung-Woo Kim, Jun Sung Moon, Yin Young Lee, Nan Hee Cho, Ji-Hyun Lee, Jae-Han Jeon, Yeon-Kyung Choi, Mi Kyung Kim, Keun-Gyu Park
- Diabetes Metab J. 2021;45(1):109-114. Published online December 4, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0226

- 9,422 View
- 307 Download
- 23 Web of Science
- 24 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
- This study investigated the impact of social distancing due to coronavirus disease 2019 (COVID-19) on glycemic control in people with type 2 diabetes mellitus (T2DM). We retrospectively analyzed the change in glycosylated hemoglobin level (ΔHbA1c) in people with T2DM who undertook social distancing because of COVID-19. We compared the ΔHbA1c between COVID-19 and non-COVID-19 cohorts that were enrolled at the same time of year. The ΔHbA1c of the COVID-19 cohort was significantly higher than that of two non-COVID-19 cohorts. Subgroup analysis according to age and baseline HbA1c level showed that social distancing significantly increased the mean HbA1c level of participants of <50 years. The ΔHbA1c of participants of <50 years and with HbA1c <7.0% in the COVID-19 cohort showed larger changes than other subgroups. In adjusted model, adjusted ΔHbA1c levels in the COVID-19 cohort remained significantly higher than those in the two other cohorts. Social distancing negatively impacts blood glucose control in people with T2DM, especially those who are younger and have good blood glucose control.
-
Citations
Citations to this article as recorded by- Impact of two COVID-19 lockdowns on HbA1c levels in patients with type 2 diabetes and associations with patient characteristics: a multicentre, observational cohort study over three years
Ingmar Schäfer, Daniel Tajdar, Laura Walther, Lasse Bittner, Dagmar Lühmann, Martin Scherer
Frontiers in Public Health.2024;[Epub] CrossRef - Influence of the COVID-19 pandemic on the achievement of guideline targets for HbA1c, blood pressure, and LDL cholesterol in people with diabetes in Japan
Shingo Kuwajima, Takahito Itoh, Tatsuya Sato, Shoya Ino, Satoru Shibata, Kouhei Ohno, Hiroyuki Hotta, Tomoaki Matsumoto, Hitoshi Ooiwa, Hirofumi Kubo, Takayuki Miki
Diabetology International.2024;[Epub] CrossRef - Socioeconomic status and the effect of prolonged pandemic confinement on anthropometric and glycaemic outcomes in adults with type 2 diabetes mellitus
Chandana Wijeweera, Ummul Muhfaza, Reginald V. Lord, Peter Petocz, Juliana Chen, Veronica Preda
Primary Care Diabetes.2024;[Epub] CrossRef - Physical and Mental Health Characteristics of Hospitalized COVID-19 Patients with and without Type 2 Diabetes Mellitus in Turkey
Abdulbari Bener, Murat Atmaca, Abdulla O. A. A. Al-Hamaq, Antonio Ventriglio
Brain Sciences.2024; 14(4): 377. CrossRef - Self-Care of Adults with Type 2 Diabetes During the COVID-19 Pandemic: A Qualitative Interpretive Description Study
Michela Luciani, Camilla Bigoni, Marta Canesi, Matteo Masotto, Diletta Fabrizi, Stefania Di Mauro, Davide Ausili
Clinical Nursing Research.2023; 32(1): 73. CrossRef - Changes in body weight and glycemic control in association with COVID-19 Shutdown among 23,000 adults with type 2 diabetes
Emily Panza, Kevin E. Kip, Kripa Venkatakrishnan, Oscar C. Marroquin, Rena R. Wing
Acta Diabetologica.2023; 60(6): 787. CrossRef - The Impact of a Lockdown for the COVID-19 Pandemic on Seasonal HbA1c Variation in Patients with Type 2 Diabetes
Yu-Cheng Cheng, Yu-Hsuan Li, Hsiu-Chen Liu, Chiann-Yi Hsu, Wan-Jen Chang, I-Te Lee, Chin-Li Lu
Life.2023; 13(3): 763. CrossRef - Changes in the mean incidence and variance of orthopedic diseases before and during the COVID-19 pandemic in Korea: a retrospective study
Joo-Hee Kim, Mi Jung Kwon, Hyo Geun Choi, Sang Jun Lee, Sangwon Hwang, Jaemin Lee, San-Hui Lee, Jung Woo Lee
BMC Musculoskeletal Disorders.2023;[Epub] CrossRef - Gender differences-based bioinformatics analysis to identify hub genes and key pathways in type 2 diabetes
Md Sojib Hossain, Subrina Islam Rupa, Md Sumon Sarkar, Md Al Amin, Mst Tania Khatun, Md Shamim, Md Zahidul Islam
Informatics in Medicine Unlocked.2023; 40: 101302. CrossRef - Retrospective Study on the Impact of COVID-19 Lockdown on Patients with Type 2 Diabetes in Northern Taiwan
Hsuan Huang, Hsiao-Ling Su, Chih-Hsung Huang, Yi-Hsin Lin
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 2539. CrossRef - Understanding impacts of COVID-19 restrictions on glycemic control for patients with diabetes in Japan
Kiyoko Uno-Eder, Noriko Satoh-Asahara, Manabu Hibiya, Kenji Uno, Takuya Uchino, Koji Morita, Toshio Ishikawa, Tetsuji Kaneko, Hajime Yamakage, Yuki Kitaoka, Tomohiro Sawa, Kazuhisa Tsukamoto, Tamio Teramoto
Journal of Diabetes & Metabolic Disorders.2023; 22(2): 1695. CrossRef - Impacts of the COVID-19 pandemic on unmet social needs, self-care, and outcomes among people with diabetes and poor glycemic control
Minal R. Patel, Guanghao Zhang, Cindy Leung, Peter X.K. Song, Michele Heisler, Hae Mi Choe, Roshanak Mehdipanah, Xu Shi, Kenneth Resnicow, Geila Rajaee, John D. Piette
Primary Care Diabetes.2022; 16(1): 57. CrossRef - Impact of the COVID-19 Pandemic on Glycemic Control and Blood Pressure Control in Patients with Diabetes in Japan
Keisuke Endo, Takayuki Miki, Takahito Itoh, Hirofumi Kubo, Ryosuke Ito, Kouhei Ohno, Hiroyuki Hotta, Nobuo Kato, Tomoaki Matsumoto, Aya Kitamura, Mai Tamayama, Takako Wataya, Ayaka Yamaya, Rei Ishikawa, Hitoshi Ooiwa
Internal Medicine.2022; 61(1): 37. CrossRef - The Effects of COVID-19 Lockdown on Glycaemic Control and Lipid Profile in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis
Omorogieva Ojo, Xiao-Hua Wang, Osarhumwese Osaretin Ojo, Edith Orjih, Nivedita Pavithran, Amanda Rodrigues Amorim Adegboye, Qian-Qian Feng, Paul McCrone
International Journal of Environmental Research and Public Health.2022; 19(3): 1095. CrossRef - Lifestyles Under Lockdown: A Scoping Review of International Studies on Type 2 Diabetes Self-Management Behaviors During COVID-19
Caroline Cummings, Kagnica Seng, Ryan Tweet, Julie Wagner
Frontiers in Clinical Diabetes and Healthcare.2022;[Epub] CrossRef - Substitution of telemedicine for clinic visit during the COVID‐19 pandemic of 2020: Comparison of telemedicine and clinic visit
Yukiko Onishi, Rieko Ichihashi, Yoko Yoshida, Tazu Tahara, Takako Kikuchi, Toshiko Kobori, Tetsuya Kubota, Masahiko Iwamoto, Shoko Hamano, Masato Kasuga
Journal of Diabetes Investigation.2022; 13(9): 1617. CrossRef - The impact of the COVID-19 pandemic on the management of patients with chronic diseases in Primary Health Care
Panagiotis Stachteas, Manolis Symvoulakis, Apostolos Tsapas, Emmanouil Smyrnakis
Population Medicine.2022; 4(August): 1. CrossRef - Effects of COVID-19 Pandemic and Lockdown on Monitoring and Treatment Balance of Finnish Coronary Heart Disease and Type 2 Diabetes Patients
Piia Lavikainen, Marja-Leena Lamidi, Teppo Repo, Laura Inglin, Janne Martikainen, Tiina Laatikainen
Clinical Epidemiology.2022; Volume 14: 1363. CrossRef - Impact of Social Distancing Due to Coronavirus Disease 2019 on the Changes in Glycosylated Hemoglobin Level in People with Type 2 Diabetes Mellitus (Diabetes Metab J 2021;45:109-14)
Junghyun Noh
Diabetes & Metabolism Journal.2021; 45(2): 275. CrossRef - Impact of Social Distancing Due to Coronavirus Disease 2019 on the Changes in Glycosylated Hemoglobin Level in People with Type 2 Diabetes Mellitus (Diabetes Metab J 2021;45:109-14)
Sung-Don Park, Sung-Woo Kim, Jun Sung Moon, Jae-Han Jeon, Mi Kyung Kim, Keun-Gyu Park
Diabetes & Metabolism Journal.2021; 45(2): 279. CrossRef - Glucose control in diabetes during home confinement for the first pandemic wave of COVID-19: a meta-analysis of observational studies
Giovanni Antonio Silverii, Chiara Delli Poggi, Ilaria Dicembrini, Matteo Monami, Edoardo Mannucci
Acta Diabetologica.2021; 58(12): 1603. CrossRef - The impact of COVID-19 pandemic on glycemic control in patients with diabetes mellitus in Turkey: a multi-center study from Kocaeli
Alev Selek, Emre Gezer, Eda Altun, Mehmet Sözen, Ömercan Topaloğlu, Damla Köksalan, Halil Demirkan, Dilek Karakaya, Berrin Cetinarslan, Zeynep Cantürk, Dilek Taymez
Journal of Diabetes & Metabolic Disorders.2021; 20(2): 1461. CrossRef - Effects of Social Distancing on Diabetes Management in Older Adults during COVID-19 Pandemic
Soo Myoung Shin, Tae Jung Oh, Sung Hee Choi, Hak Chul Jang
Diabetes & Metabolism Journal.2021; 45(5): 765. CrossRef - Year-Long Trend in Glycated Hemoglobin Levels in Patients with Type 2 Diabetes during the COVID-19 Pandemic
Jonghwa Jin, Seong Wook Lee, Won-Ki Lee, Jae-Han Jeon, Jung-Guk Kim, In-Kyu Lee, Yeon-Kyung Choi, Keun-Gyu Park
Endocrinology and Metabolism.2021; 36(5): 1142. CrossRef
- Impact of two COVID-19 lockdowns on HbA1c levels in patients with type 2 diabetes and associations with patient characteristics: a multicentre, observational cohort study over three years
- Covid-19
-
- The Clinical Characteristics and Outcomes of Patients with Moderate-to-Severe Coronavirus Disease 2019 Infection and Diabetes in Daegu, South Korea
- Mi Kyung Kim, Jae-Han Jeon, Sung-Woo Kim, Jun Sung Moon, Nan Hee Cho, Eugene Han, Ji Hong You, Ji Yeon Lee, Miri Hyun, Jae Seok Park, Yong Shik Kwon, Yeon-Kyung Choi, Ki Tae Kwon, Shin Yup Lee, Eon Ju Jeon, Jin-Woo Kim, Hyo-Lim Hong, Hyun Hee Kwon, Chi Young Jung, Yin Young Lee, Eunyeoung Ha, Seung Min Chung, Jian Hur, June Hong Ahn, Na-young Kim, Shin-Woo Kim, Hyun Ha Chang, Yong Hoon Lee, Jaehee Lee, Keun-Gyu Park, Hyun Ah Kim, Ji-Hyun Lee
- Diabetes Metab J. 2020;44(4):602-613. Published online August 12, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0146
- 13,306 View
- 206 Download
- 67 Web of Science
- 74 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
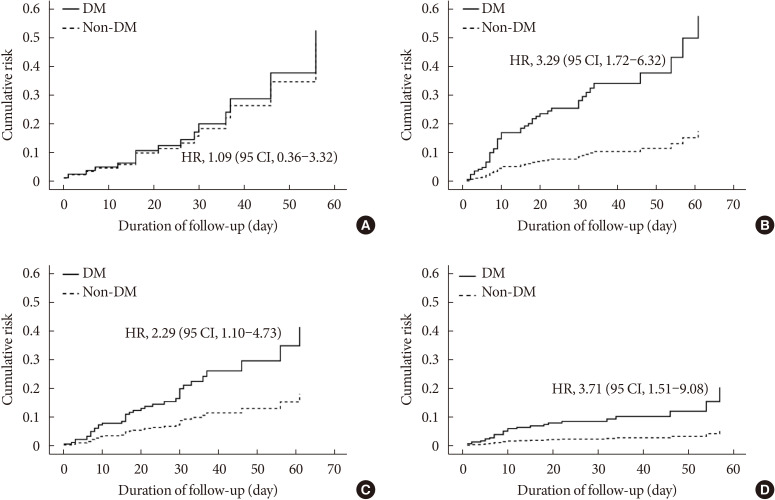
ePub Background Coronavirus disease 2019 (COVID-19) is a global pandemic that had affected more than eight million people worldwide by June 2020. Given the importance of the presence of diabetes mellitus (DM) for host immunity, we retrospectively evaluated the clinical characteristics and outcomes of moderate-to-severe COVID-19 in patients with diabetes.
Methods We conducted a multi-center observational study of 1,082 adult inpatients (aged ≥18 years) who were admitted to one of five university hospitals in Daegu because of the severity of their COVID-19-related disease. The demographic, laboratory, and radiologic findings, and the mortality, prevalence of severe disease, and duration of quarantine were compared between patients with and without DM. In addition, 1:1 propensity score (PS)-matching was conducted with the DM group.
Results Compared with the non-DM group (
n =847), patients with DM (n =235) were older, exhibited higher mortality, and required more intensive care. Even after PS-matching, patients with DM exhibited more severe disease, and DM remained a prognostic factor for higher mortality (hazard ratio, 2.40; 95% confidence interval, 1.38 to 4.15). Subgroup analysis revealed that the presence of DM was associated with higher mortality, especially in older people (≥70 years old). Prior use of a dipeptidyl peptidase-4 inhibitor or a renin-angiotensin system inhibitor did not affect mortality or the clinical severity of the disease.Conclusion DM is a significant risk factor for COVID-19 severity and mortality. Our findings imply that COVID-19 patients with DM, especially if elderly, require special attention and prompt intensive care.
-
Citations
Citations to this article as recorded by- Potential use of sodium glucose co-transporter 2 inhibitors during acute illness: a systematic review based on COVID-19
Carmen Tisch, Eleni Xourgia, Aristomenis Exadaktylos, Mairi Ziaka
Endocrine.2024;[Epub] CrossRef - Insulin and Metformin Administration: Unravelling the Multifaceted Association with Mortality across Various Clinical Settings Considering Type 2 Diabetes Mellitus and COVID-19
Łukasz Lewandowski, Agnieszka Bronowicka-Szydełko, Maciej Rabczyński, Dorota Bednarska-Chabowska, Joanna Adamiec-Mroczek, Adrian Doroszko, Małgorzata Trocha, Krzysztof Kujawa, Agnieszka Matera-Witkiewicz, Edwin Kuźnik, Paweł Lubieniecki, Marcin Madziarski
Biomedicines.2024; 12(3): 605. CrossRef - Pre-admission use of sodium glucose transporter-2 inhibitor (SGLT-2i) may significantly improves Covid-19 outcomes in patients with diabetes: A systematic review, meta-analysis, and meta-regression
Hikmat Permana, Theo Audi Yanto, Timotius Ivan Hariyanto
Diabetes Research and Clinical Practice.2023; 195: 110205. CrossRef - Risk phenotypes of diabetes and association with COVID-19 severity and death: an update of a living systematic review and meta-analysis
Sabrina Schlesinger, Alexander Lang, Nikoletta Christodoulou, Philipp Linnerz, Kalliopi Pafili, Oliver Kuss, Christian Herder, Manuela Neuenschwander, Janett Barbaresko, Michael Roden
Diabetologia.2023; 66(8): 1395. CrossRef - Factors influencing the severity of COVID-19 course for patients with diabetes mellitus in tashkent: a retrospective cohort study
A. V. Alieva, A. A. Djalilov, F. A. Khaydarova, A. V. Alimov, D. Z. Khalilova, V. A. Talenova, N. U. Alimova, M. D. Aripova, A. S. Sadikova
Obesity and metabolism.2023; 20(2): 92. CrossRef - Pituitary Diseases and COVID-19 Outcomes in South Korea: A Nationwide Cohort Study
Jeonghoon Ha, Kyoung Min Kim, Dong-Jun Lim, Keeho Song, Gi Hyeon Seo
Journal of Clinical Medicine.2023; 12(14): 4799. CrossRef - Epidemiological features and consequences of COVID‐19 in patients with and without gastrointestinal symptoms in southwestern Iran. A retrospective observational study
Habibollah Azarbakhsh, Leila Moftakhar, Aliasghar Valipour, Alireza Mirahmadizadeh, Hekmat Allah Moradi, Elahe Piraee
Health Science Reports.2023;[Epub] CrossRef - The Impact of Long-Term Conditions and Comorbidity Patterns on COVID-19 Infection and Hospitalisation: A Cohort Study
Yun-Ting Huang, Andrew Steptoe, Riyaz S. Patel, Esme Fuller Thomson, Dorina Cadar
Gerontology.2023; 69(10): 1200. CrossRef - Association Between Anti-diabetic Agents and Clinical Outcomes of COVID-19 in Patients with Diabetes: A Systematic Review and Meta-Analysis
Tiantian Han, Shaodi Ma, Chenyu Sun, Huimei Zhang, Guangbo Qu, Yue Chen, Ce Cheng, Eric L. Chen, Mubashir Ayaz Ahmed, Keun Young Kim, Raveena Manem, Mengshi Chen, Zhichun Guo, Hongru Yang, Yue Yan, Qin Zhou
Archives of Medical Research.2022; 53(2): 186. CrossRef - Use of DPP4i reduced odds of clinical deterioration and hyperinflammatory syndrome in COVID-19 patients with type 2 diabetes: Propensity score analysis of a territory-wide cohort in Hong Kong
Carlos K.H. Wong, David T.W. Lui, Angel Y.C. Lui, Ashley C.Y. Kwok, Marshall C.H. Low, Kristy T.K. Lau, Ivan C.H. Au, Xi Xiong, Matthew S.H. Chung, Eric H.Y. Lau, Benjamin J. Cowling
Diabetes & Metabolism.2022; 48(1): 101307. CrossRef - Dipeptidyl peptidase-4 (DPP-IV) inhibitor was associated with mortality reduction in COVID-19 — A systematic review and meta-analysis
Ahmad Fariz Malvi Zamzam Zein, Wilson Matthew Raffaello
Primary Care Diabetes.2022; 16(1): 162. CrossRef - Prevalence and impact of diabetes in hospitalized COVID‐19 patients: A systematic review and meta‐analysis
Sian A. Bradley, Maciej Banach, Negman Alvarado, Ivica Smokovski, Sonu M. M. Bhaskar
Journal of Diabetes.2022; 14(2): 144. CrossRef - Interplay between Inflammaging, Frailty and Nutrition in Covid-19: Preventive and Adjuvant Treatment Perspectives
A. Padilha de Lima, M. Macedo Rogero, T. Araujo Viel, H.M. Garay-Malpartida, I. Aprahamian, Sandra Maria Lima Ribeiro
The Journal of nutrition, health and aging.2022; 26(1): 67. CrossRef - Increase in blood glucose level and incidence of diabetic ketoacidosis in children with type 1 diabetes mellitus in the Daegu-Gyeongbuk area during the coronavirus disease 2019 (COVID-19) pandemic: a retrospective cross-sectional study
Mi Seon Lee, Rosie Lee, Cheol Woo Ko, Jung Eun Moon
Journal of Yeungnam Medical Science.2022; 39(1): 46. CrossRef - Interrelationship between 2019-nCov receptor DPP4 and diabetes mellitus targets based on protein interaction network
Qian Gao, Wenjun Zhang, Tingting Li, Guojun Yang, Wei Zhu, Naijun Chen, Huawei Jin
Scientific Reports.2022;[Epub] CrossRef - Can sodium-glucose co-transporter-2 (SGLT-2) inhibitor reduce the risk of adverse complications due to COVID-19? – Targeting hyperinflammation
Afnan Alshnbari, Iskandar Idris
Current Medical Research and Opinion.2022; 38(3): 357. CrossRef - Commentary: Mortality Risk of Antidiabetic Agents for Type 2 Diabetes With COVID-19: A Systematic Review and Meta-Analysis
Li-Min Zhao, Xie-Hui Chen, Mei Qiu
Frontiers in Endocrinology.2022;[Epub] CrossRef - COVID-19 and Diabetes
Awadhesh Kumar Singh, Kamlesh Khunti
Annual Review of Medicine.2022; 73(1): 129. CrossRef - The enzymes in COVID-19: A review
Maria Helena Menezes Estevam Alves, Layla Carvalho Mahnke, Tifany Cerqueira Macedo, Thais Ketinly dos Santos Silva, Luiz Bezerra Carvalho Junior
Biochimie.2022; 197: 38. CrossRef - IMPACT OF ANTIDIABETIC DRUGS ON RISK AND OUTCOME OF COVID-19 INFECTION: A REVIEW
Adnan A. Zainal, Marwan M. Merkhan
Military Medical Science Letters.2022; 91(2): 140. CrossRef - Does metformin affect outcomes in COVID‐19 patients with new or pre‐existing diabetes mellitus? A systematic review and meta‐analysis
Adithan Ganesh, Michael D. Randall
British Journal of Clinical Pharmacology.2022; 88(6): 2642. CrossRef - Diabetes, Metformin and the Clinical Course of Covid-19: Outcomes, Mechanisms and Suggestions on the Therapeutic Use of Metformin
Clifford J. Bailey, Mike Gwilt
Frontiers in Pharmacology.2022;[Epub] CrossRef - The Role of Diabetes and Hyperglycemia on COVID-19 Infection Course—A Narrative Review
Evangelia Tzeravini, Eleftherios Stratigakos, Chris Siafarikas, Anastasios Tentolouris, Nikolaos Tentolouris
Frontiers in Clinical Diabetes and Healthcare.2022;[Epub] CrossRef - Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: A meta-analysis
Nam Nhat Nguyen, Dung Si Ho, Hung Song Nguyen, Dang Khanh Ngan Ho, Hung-Yuan Li, Chia-Yuan Lin, Hsiao-Yean Chiu, Yang-Ching Chen
Metabolism.2022; 131: 155196. CrossRef - Glucose-Lowering Agents and COVID-19
Ah Reum Khang
The Journal of Korean Diabetes.2022; 23(1): 1. CrossRef - Impact of diabetes on COVID‐19 mortality and hospital outcomes from a global perspective: An umbrella systematic review and meta‐analysis
Stavroula Kastora, Manisha Patel, Ben Carter, Mirela Delibegovic, Phyo Kyaw Myint
Endocrinology, Diabetes & Metabolism.2022;[Epub] CrossRef - The Association Between Antidiabetic Agents and Clinical Outcomes of COVID-19 Patients With Diabetes: A Bayesian Network Meta-Analysis
Yidan Chen, Xingfei Lv, Sang Lin, Mohammad Arshad, Mengjun Dai
Frontiers in Endocrinology.2022;[Epub] CrossRef - Renin‐Angiotensin Aldosterone System Inhibitors and COVID‐19: A Systematic Review and Meta‐Analysis Revealing Critical Bias Across a Body of Observational Research
Jordan Loader, Frances C. Taylor, Erik Lampa, Johan Sundström
Journal of the American Heart Association.2022;[Epub] CrossRef - Diabetes and SARS-CoV-2–Is There a Mutual Connection?
Anna P. Jedrzejak, Edyta K. Urbaniak, Jadwiga A. Wasko, Natalia Ziojla, Malgorzata Borowiak
Frontiers in Cell and Developmental Biology.2022;[Epub] CrossRef - The relationship of age, sex and prothrombin time related to the severity and mortality of COVID-19 patients with diabetes mellitus: a systematic review and meta analysis
Audrey Fabianisa Mirza, Ceria Halim, Mutiara Indah Sari
F1000Research.2022; 11: 729. CrossRef - Are lipid ratios and triglyceride-glucose index associated with critical care outcomes in COVID-19 patients?
Marzieh Rohani-Rasaf, Kosar Mirjalili, Akram Vatannejad, Maryam Teimouri, Xiao-Feng Yang
PLOS ONE.2022; 17(8): e0272000. CrossRef - Early glycaemic variability increases 28-day mortality and prolongs intensive care unit stay in critically ill patients with pneumonia
Seong Ho Kim, Ji Young Kim, Eun Song Kim, Il Rae Park, Eun Yeong Ha, Seung Min Chung, Jun Sung Moon, Ji Sung Yoon, Kyu Chang Won, Hyoung Woo Lee
Annals of Medicine.2022; 54(1): 2724. CrossRef - Dipeptidyl peptidase 4 inhibitors in COVID-19: Beyond glycemic control
Niya Narayanan, Dukhabandhu Naik, Jayaprakash Sahoo, Sadishkumar Kamalanathan
World Journal of Virology.2022; 11(6): 399. CrossRef - Prevalencia de secuelas en pacientes con diabetes mellitus tipo 2 sobrevivientes al COVID-19
Gianela M. Cancino-Castillo, Miguel A. Tresierra-Ayala, Jorge L. Campos-Reyna, Jaime Rosales-Rimache
REVISTA MÉDICA VALLEJIANA/ Vallejian Medical Journal.2022; 11(2): 48. CrossRef - Predictors of adverse in-hospital outcome and recovery in patients with diabetes mellitus and COVID-19 pneumonia in Iraq
Hussein Nafakhi, Mohammed Alareedh, Karrar Al-Buthabhak, Foaad Shaghee, Ahmed Nafakhi, Samet Kasim
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2021; 15(1): 33. CrossRef - Non-insulin anti-diabetic agents in patients with type 2 diabetes and COVID-19: A Critical Appraisal of Literature
Awadhesh Kumar Singh, Ritu Singh, Banshi Saboo, Anoop Misra
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2021; 15(1): 159. CrossRef - COVID-19 associated with diabetes and other noncommunicable diseases led to a global health crisis
Mark Thomaz Ugliara Barone, Belinda Ngongo, Simone Bega Harnik, Lucas Xavier de Oliveira, Dániel Végh, Patrícia Vieira de Luca, Hermelinda Cordeiro Pedrosa, Franco Giraudo, Roque Cardona-Hernandez, Nayanjeet Chaudhury, Luiz Menna-Barreto
Diabetes Research and Clinical Practice.2021; 171: 108587. CrossRef - A meta-analysis on the preadmission use of DPP-4 inhibitors and risk of a fatal or severe course of illness in patients with COVID-19
Chia Siang Kow, Syed Shahzad Hasan
Therapies.2021; 76(4): 361. CrossRef - Disentangling conflicting evidence on DPP-4 inhibitors and outcomes of COVID-19: narrative review and meta-analysis
B. M. Bonora, A. Avogaro, G. P. Fadini
Journal of Endocrinological Investigation.2021; 44(7): 1379. CrossRef - Prognostic bioindicators in severe COVID-19 patients
L. Bergantini, E. Bargagli, M. d'Alessandro, R.M. Refini, P. Cameli, L. Galasso, C. Scapellato, F. Montagnani, S. Scolletta, F. Franchi, S. Valente, D. Bennett, G. Sebastiani, B. Frediani, F. Dotta
Cytokine.2021; 141: 155455. CrossRef - Epidemiological characteristics and outcomes of COVID-19 in diabetic versus non-diabetic patients
Leila Moftakhar, Parisa Moftakhar, Elahe Piraee, Haleh Ghaem, Aliasghar Valipour, Habibollah Azarbakhsh
International Journal of Diabetes in Developing Countries.2021; 41(3): 383. CrossRef - DPP-4 inhibition and COVID-19: From initial concerns to recent expectations
André J. Scheen
Diabetes & Metabolism.2021; 47(2): 101213. CrossRef - Use of dipeptidyl peptidase‐4 inhibitors and prognosis of COVID‐19 in hospitalized patients with type 2 diabetes: A propensity score analysis from the CORONADO study
Ronan Roussel, Patrice Darmon, Matthieu Pichelin, Thomas Goronflot, Yawa Abouleka, Leila Ait Bachir, Ingrid Allix, Deborah Ancelle, Sara Barraud, Lyse Bordier, Aurélie Carlier, Nicolas Chevalier, Christine Coffin‐Boutreux, Emmanuel Cosson, Anne Dorange, O
Diabetes, Obesity and Metabolism.2021; 23(5): 1162. CrossRef - Dipeptidyl peptidase-4 inhibitor use and mortality in COVID-19 patients with diabetes mellitus: an updated systematic review and meta-analysis
Rimesh Pal, Mainak Banerjee, Soham Mukherjee, Ranjitpal Singh Bhogal, Amanpreet Kaur, Sanjay K. Bhadada
Therapeutic Advances in Endocrinology and Metabolism.2021; 12: 204201882199648. CrossRef - Renin–angiotensin-system inhibitors and all-cause mortality in patients with COVID-19: a systematic review and meta-analysis of observational studies
Chirag Bavishi, Paul K. Whelton, Giuseppe Mancia, Giovanni Corrao, Franz H. Messerli
Journal of Hypertension.2021; 39(4): 784. CrossRef - Evaluation of the Current Therapeutic Approaches for COVID-19: A Systematic Review and a Meta-analysis
Zeinab Abdelrahman, Qian Liu, Shanmei Jiang, Mengyuan Li, Qingrong Sun, Yue Zhang, Xiaosheng Wang
Frontiers in Pharmacology.2021;[Epub] CrossRef - Dipeptidyl peptidase 4 (DPP4) inhibitor and outcome from coronavirus disease 2019 (COVID-19) in diabetic patients: a systematic review, meta-analysis, and meta-regression
Timotius Ivan Hariyanto, Andree Kurniawan
Journal of Diabetes & Metabolic Disorders.2021; 20(1): 543. CrossRef - Impact of diabetes mellitus on in-hospital mortality in adult patients with COVID-19: a systematic review and meta-analysis
Halla Kaminska, Lukasz Szarpak, Dariusz Kosior, Wojciech Wieczorek, Agnieszka Szarpak, Mahdi Al-Jeabory, Wladyslaw Gawel, Aleksandra Gasecka, Milosz J. Jaguszewski, Przemyslawa Jarosz-Chobot
Acta Diabetologica.2021; 58(8): 1101. CrossRef - Dipeptidyl peptidase-4 (DPP-4) inhibitor and mortality in coronavirus disease 2019 (COVID-19) – A systematic review, meta-analysis, and meta-regression
Iis Inayati Rakhmat, Yudith Yunia Kusmala, Dewi Ratih Handayani, Henny Juliastuti, Eka Noneng Nawangsih, Arief Wibowo, Michael Anthonius Lim, Raymond Pranata
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2021; 15(3): 777. CrossRef - Post-infection depressive, anxiety and post-traumatic stress symptoms: A prospective cohort study in patients with mild COVID-19
Flavia Ismael, João C.S. Bizario, Tatiane Battagin, Beatriz Zaramella, Fabio E. Leal, Julio Torales, Antonio Ventriglio, Megan E. Marziali, Silvia S. Martins, João M. Castaldelli-Maia
Progress in Neuro-Psychopharmacology and Biological Psychiatry.2021; 111: 110341. CrossRef - Managing diabetes in diabetic patients with COVID: where do we start from?
Angelo Avogaro, Benedetta Bonora, Gian Paolo Fadini
Acta Diabetologica.2021; 58(11): 1441. CrossRef - Is diabetes mellitus a wrongdoer to COVID-19 severity?
Sanjib Sarkar, Dibyendu Das, Sawlang Borsingh Wann, Jatin Kalita, Prasenjit Manna
Diabetes Research and Clinical Practice.2021; 178: 108936. CrossRef - Dipeptidyl Peptidase 4 Inhibitor, an Update
Ju Hee Lee
The Journal of Korean Diabetes.2021; 22(2): 91. CrossRef - Correlation Analysis Between Serum Uric Acid, Prealbumin Level, Lactate Dehydrogenase, and Severity of COVID-19
Zhenmu Jin, Mo Zheng, Jichan Shi, Xinchun Ye, Fang Cheng, Que-Lu Chen, Jianping Huang, Xian-Gao Jiang
Frontiers in Molecular Biosciences.2021;[Epub] CrossRef - Association Between Glucagon-Like Peptide 1 Receptor Agonist and Sodium–Glucose Cotransporter 2 Inhibitor Use and COVID-19 Outcomes
Anna R. Kahkoska, Trine Julie Abrahamsen, G. Caleb Alexander, Tellen D. Bennett, Christopher G. Chute, Melissa A. Haendel, Klara R. Klein, Hemalkumar Mehta, Joshua D. Miller, Richard A. Moffitt, Til Stürmer, Kajsa Kvist, John B. Buse, Tim Q. Duong
Diabetes Care.2021; 44(7): 1564. CrossRef - The effect of metformin on mortality and severity in COVID-19 patients with diabetes mellitus
Wenxing Yang, Xuehong Sun, Jun Zhang, Kui Zhang
Diabetes Research and Clinical Practice.2021; 178: 108977. CrossRef - Renin‐Angiotensin Aldosterone System Inhibitors in Primary Prevention and COVID‐19
Jordan Loader, Erik Lampa, Stefan Gustafsson, Thomas Cars, Johan Sundström
Journal of the American Heart Association.2021;[Epub] CrossRef - Factors influencing on development of COVID-19 pneumonia and association with oral anti-diabetic drugs in hospitalized patients with diabetes mellitus
Ayça Elibol, Didem Eren, Macide Deniz Erdoğan, Merve Elmaağaç, Oguzhan Sıtkı Dizdar, İlhami Çelik, Ali İhsan Günal
Primary Care Diabetes.2021; 15(5): 806. CrossRef - Aging & COVID-19 susceptibility, disease severity, and clinical outcomes: The role of entangled risk factors
Melina Farshbafnadi, Sara Kamali Zonouzi, Mohammadmahdi Sabahi, Mahsa Dolatshahi, Mohammad Hadi Aarabi
Experimental Gerontology.2021; 154: 111507. CrossRef - Classical and Counter-Regulatory Renin–Angiotensin System: Potential Key Roles in COVID-19 Pathophysiology
Moudhi Almutlaq, Abir Abdullah Alamro, Fayhan Alroqi, Tlili Barhoumi
CJC Open.2021; 3(8): 1060. CrossRef - Metformin in Patients With COVID-19: A Systematic Review and Meta-Analysis
Yin Li, Xue Yang, Peijing Yan, Tong Sun, Zhi Zeng, Sheyu Li
Frontiers in Medicine.2021;[Epub] CrossRef - Pre-existing health conditions and severe COVID-19 outcomes: an umbrella review approach and meta-analysis of global evidence
Marina Treskova-Schwarzbach, Laura Haas, Sarah Reda, Antonia Pilic, Anna Borodova, Kasra Karimi, Judith Koch, Teresa Nygren, Stefan Scholz, Viktoria Schönfeld, Sabine Vygen-Bonnet, Ole Wichmann, Thomas Harder
BMC Medicine.2021;[Epub] CrossRef - COVID-19 Vaccination for Endocrine Patients: A Position Statement from the Korean Endocrine Society
Cheol Ryong Ku, Kyong Yeun Jung, Chang Ho Ahn, Jun Sung Moon, Ju Hee Lee, Eun Heui Kim, Hyemi Kwon, Hee Kyung Kim, Sunghwan Suh, Sangmo Hong, Jeonghoon Ha, Eun Roh, Jin Hwa Kim, Mi-kyung Kim
Endocrinology and Metabolism.2021; 36(4): 757. CrossRef - High Fibrosis-4 Index Is Related with Worse Clinical Outcome in Patients with Coronavirus Disease 2019 and Diabetes Mellitus: A Multicenter Observational Study
Sung-Woo Kim, Jae-Han Jeon, Jun Sung Moon, Mi Kyung Kim
Endocrinology and Metabolism.2021; 36(4): 800. CrossRef - Mortality Risk of Antidiabetic Agents for Type 2 Diabetes With COVID-19: A Systematic Review and Meta-Analysis
Chengxia Kan, Yang Zhang, Fang Han, Qian Xu, Tongtong Ye, Ningning Hou, Xiaodong Sun
Frontiers in Endocrinology.2021;[Epub] CrossRef - Analysis of influence of background therapy for comorbidities in the period before infection on the risk of the lethal COVID outcome. Data from the international ACTIV SARS-CoV-2 registry («Analysis of chronic non-infectious diseases dynamics after COVID-
E. I. Tarlovskaya, A. G. Arutyunov, A. O. Konradi, Yu. M. Lopatin, A. P. Rebrov, S. N. Tereshchenko, A. I. Chesnikova, H. G. Hayrapetyan, A. P. Babin, I. G. Bakulin, N. V. Bakulina, L. A. Balykova, A. S. Blagonravova, M. V. Boldina, A. R. Vaisberg, A. S.
Kardiologiia.2021; 61(9): 20. CrossRef - Association of clinical characteristics, antidiabetic and cardiovascular agents with diabetes mellitus and COVID-19: a 7-month follow-up cohort study
Marzieh Pazoki, Fatemeh Chichagi, Azar Hadadi, Samira Kafan, Mahnaz Montazeri, Sina Kazemian, Arya Aminorroaya, Mehdi Ebrahimi, Haleh Ashraf, Mojgan Mirabdolhagh Hazaveh, Mohammad Reza Khajavi, Reza Shariat Moharari, Seyed Hamidreza Sharifnia, Shahrokh Ka
Journal of Diabetes & Metabolic Disorders.2021; 20(2): 1545. CrossRef - COVID-19 and Diabetes: A Comprehensive Review of Angiotensin Converting Enzyme 2, Mutual Effects and Pharmacotherapy
Lingli Xie, Ziying Zhang, Qian Wang, Yangwen Chen, Dexue Lu, Weihua Wu
Frontiers in Endocrinology.2021;[Epub] CrossRef - Impact of Diabetes on COVID-19 Mortality and Hospital Outcomes, a Global Perspective: An ONTOP Systematic Review and Meta-Analysis
Stavroula Kastora, Manisha Patel, Ben Carter, Mirela Delibegovic, Phyo Kyaw Myint
SSRN Electronic Journal .2021;[Epub] CrossRef - Decision Trees: Predictions of Global Vulnerability to Coronavirus Outbreaks
Moacir José da Silva
SSRN Electronic Journal .2020;[Epub] CrossRef - The potential association between common comorbidities and severity and mortality of coronavirus disease 2019: A pooled analysis
Liman Luo, Menglu Fu, Yuanyuan Li, Shuiqing Hu, Jinlan Luo, Zhihui Chen, Jing Yu, Wenhua Li, Ruolan Dong, Yan Yang, Ling Tu, Xizhen Xu
Clinical Cardiology.2020; 43(12): 1478. CrossRef - The Effect of Metformin Consumption on Mortality in Hospitalized COVID-19 patients: a systematic review and meta-analysis
Antonia Anna Lukito, Raymond Pranata, Joshua Henrina, Michael Anthonius Lim, Sherly Lawrensia, Ketut Suastika
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2020; 14(6): 2177. CrossRef - Risk Factors on the Progression to Clinical Outcomes of COVID-19 Patients in South Korea: Using National Data
Seon-Rye Kim, Seoul-Hee Nam, Yu-Rin Kim
International Journal of Environmental Research and Public Health.2020; 17(23): 8847. CrossRef - Clinical Outcomes of COVID-19 Patients with Type 2 Diabetes: A Population-Based Study in Korea
Ji Hong You, Sang Ah Lee, Sung-Youn Chun, Sun Ok Song, Byung-Wan Lee, Dae Jung Kim, Edward J. Boyko
Endocrinology and Metabolism.2020; 35(4): 901. CrossRef
- Potential use of sodium glucose co-transporter 2 inhibitors during acute illness: a systematic review based on COVID-19
- Guideline/Fact Sheet
- Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Mellitus: A Position Statement of the Fatty Liver Research Group of the Korean Diabetes Association
- Byung-Wan Lee, Yong-ho Lee, Cheol-Young Park, Eun-Jung Rhee, Won-Young Lee, Nan-Hee Kim, Kyung Mook Choi, Keun-Gyu Park, Yeon-Kyung Choi, Bong-Soo Cha, Dae Ho Lee, Korean Diabetes Association (KDA) Fatty Liver Research Group
- Diabetes Metab J. 2020;44(3):382-401. Published online May 11, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0010
- 12,344 View
- 337 Download
- 42 Web of Science
- 42 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader This clinical practice position statement, a product of the Fatty Liver Research Group of the Korean Diabetes Association, proposes recommendations for the diagnosis, progression and/or severity assessment, management, and follow-up of non-alcoholic fatty liver disease (NAFLD) in patients with type 2 diabetes mellitus (T2DM). Patients with both T2DM and NAFLD have an increased risk of non-alcoholic steatohepatitis (NASH) and fibrosis and a higher risk of cardiovascular diseases and diabetic complications compared to those without NAFLD. With regards to the evaluation of patients with T2DM and NAFLD, ultrasonography-based stepwise approaches using noninvasive biomarker models such as fibrosis-4 or the NAFLD fibrosis score as well as imaging studies such as vibration-controlled transient elastography with controlled attenuation parameter or magnetic resonance imaging-proton density fat fraction are recommended. After the diagnosis of NAFLD, the stage of fibrosis needs to be assessed appropriately. For management, weight reduction achieved by lifestyle modification has proven beneficial and is recommended in combination with antidiabetic agent(s). Evidence that some antidiabetic agents improve NAFLD/NASH with fibrosis in patients with T2DM is emerging. However, there are currently no definite pharmacologic treatments for NAFLD in patients with T2DM. For specific cases, bariatric surgery may be an option if indicated.
-
Citations
Citations to this article as recorded by- A combined extract containing Schisandra chinensis (SCE) reduced hepatic triglyceride accumulation in rats fed a high-sucrose diet
Haneul Lee, Eun Young Kang, Joowon Lee, Yejin Kim, Sumin Kang, Hayoon Kim, Hyun Kyung Kim, Gyoungok Gang, Sang-gil Lee, Cao Lei, Gwang-woong Go
Food Science and Biotechnology.2024; 33(6): 1449. CrossRef - Association of non-alcoholic fatty liver disease with cardiovascular disease and all cause death in patients with type 2 diabetes mellitus: nationwide population based study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
BMJ.2024; : e076388. CrossRef - Risk Scores for Prediction of Major Cardiovascular Events in Non-Alcoholic Fatty Liver Disease: A No Man’s Land?
Liliana Gheorghe, Roxana Nemteanu, Andreea Clim, Gina Eosefina Botnariu, Irina Iuliana Costache, Alina Plesa
Life.2023; 13(4): 857. CrossRef - Increased expression of sodium-glucose cotransporter 2 and O-GlcNAcylation in hepatocytes drives non-alcoholic steatohepatitis
Hye Jin Chun, Eun Ran Kim, Minyoung Lee, Da Hyun Choi, Soo Hyun Kim, Eugene Shin, Jin-Hong Kim, Jin Won Cho, Dai Hoon Han, Bong-Soo Cha, Yong-ho Lee
Metabolism.2023; 145: 155612. CrossRef - Association between fatty liver index and risk of end-stage renal disease stratified by kidney function in patients with type 2 diabetes: A nationwide population-based study
Goh Eun Chung, Kyungdo Han, Kyu-Na Lee, Jung Ho Bae, Sun Young Yang, Su-Yeon Choi, Jeong Yoon Yim, Nam Ju Heo
Diabetes & Metabolism.2023; 49(4): 101454. CrossRef - Comparison of glucagon-like peptide-1 receptor agonists and thiazolidinediones on treating nonalcoholic fatty liver disease: A network meta-analysis
Min Jeong Park, Hayeon Kim, Myeong Gyu Kim, Kyungim Kim
Clinical and Molecular Hepatology.2023; 29(3): 693. CrossRef - Histological analysis of hypoglycemic agents on liver fibrosis in patients with non-alcoholic fatty liver disease: a systematic review
Qingxing Xie, Xiaohui Pan, Xinyue Zhang, Jinfang Ma, Ge Peng, Nanwei Tong
Chinese Medical Journal.2023; 136(16): 2014. CrossRef - Hepatotropc effects of glucose-lowering drugs: non-alcoholic fatty liver disease in focus
E. V. Uzhakova, Z. E. Zshanko, E. N. Smirnova
Experimental and Clinical Gastroenterology.2023; (6): 121. CrossRef - Complementary effects of dapagliflozin and lobeglitazone on metabolism in a diet-induced obese mouse model
Yun Kyung Lee, Tae Jung Oh, Ji In Lee, Bo Yoon Choi, Hyen Chung Cho, Hak Chul Jang, Sung Hee Choi
European Journal of Pharmacology.2023; 957: 175946. CrossRef - Hepatic T-cell senescence and exhaustion are implicated in the progression of fatty liver disease in patients with type 2 diabetes and mouse model with nonalcoholic steatohepatitis
Byeong Chang Sim, Yea Eun Kang, Sun Kyoung You, Seong Eun Lee, Ha Thi Nga, Ho Yeop Lee, Thi Linh Nguyen, Ji Sun Moon, Jingwen Tian, Hyo Ju Jang, Jeong Eun Lee, Hyon-Seung Yi
Cell Death & Disease.2023;[Epub] CrossRef - 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Jong Han Choi, Kyung Ae Lee, Joon Ho Moon, Suk Chon, Dae Jung Kim, Hyun Jin Kim, Nan Hee Kim, Ji A Seo, Mee Kyoung Kim, Jeong Hyun Lim, YoonJu Song, Ye Seul Yang, Jae Hyeon Kim, You-Bin Lee, Junghyun Noh, Kyu Yeon Hur, Jong Suk Park, Sang Youl Rhee, Hae J
Diabetes & Metabolism Journal.2023; 47(5): 575. CrossRef - Circ_0004535/miR-1827/CASP8 network involved in type 2 diabetes mellitus with nonalcoholic fatty liver disease
Min Li, Ai Zeng, Xinle Tang, Hui Xu, Wei Xiong, Yanying Guo
Scientific Reports.2023;[Epub] CrossRef - Stratification by obesity class, rather than age, can identify a higher percent of children at risk for non‐alcoholic fatty liver disease and metabolic dysfunction
Aurelia Radulescu, Adam J. Dugan, Mary Killian, Suzanna L. Attia, Marialena Mouzaki, George J. Fuchs, Rohit Kohli, Henrietta Bada, Philip A. Kern, Samir Softic
Pediatric Obesity.2022;[Epub] CrossRef - Renal Tubular Damage Marker, Urinary N-acetyl-β-D-Glucosaminidase, as a Predictive Marker of Hepatic Fibrosis in Type 2 Diabetes Mellitus
Hae Kyung Kim, Minyoung Lee, Yong-ho Lee, Eun Seok Kang, Bong-Soo Cha, Byung-Wan Lee
Diabetes & Metabolism Journal.2022; 46(1): 104. CrossRef - Dulaglutide Ameliorates Palmitic Acid-Induced Hepatic Steatosis by Activating FAM3A Signaling Pathway
Jinmi Lee, Seok-Woo Hong, Min-Jeong Kim, Sun Joon Moon, Hyemi Kwon, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
Endocrinology and Metabolism.2022; 37(1): 74. CrossRef - State-of-the-Art Overview of the Pharmacological Treatment of Non-Alcoholic Steatohepatitis
Yongin Cho, Yong-ho Lee
Endocrinology and Metabolism.2022; 37(1): 38. CrossRef - Ezetimibe combination therapy with statin for non-alcoholic fatty liver disease: an open-label randomized controlled trial (ESSENTIAL study)
Yongin Cho, Hyungjin Rhee, Young-eun Kim, Minyoung Lee, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Jin-Young Choi, Yong-ho Lee
BMC Medicine.2022;[Epub] CrossRef - Obesity is an important determinant of severity in newly defined metabolic dysfunction-associated fatty liver disease
Ji Hye Huh, Kwang Joon Kim, Seung Up Kim, Bong-Soo Cha, Byung-Wan Lee
Hepatobiliary & Pancreatic Diseases International.2022; 21(3): 241. CrossRef - Anti-Obesity and Anti-Hyperglycemic Effects of Meretrix lusoria Protamex Hydrolysate in ob/ob Mice
Min Ju Kim, Ramakrishna Chilakala, Hee Geun Jo, Seung-Jae Lee, Dong-Sung Lee, Sun Hee Cheong
International Journal of Molecular Sciences.2022; 23(7): 4015. CrossRef - The associations of hepatic steatosis and fibrosis using fatty liver index and BARD score with cardiovascular outcomes and mortality in patients with new-onset type 2 diabetes: a nationwide cohort study
Jiyun Park, Gyuri Kim, Bong-Sung Kim, Kyung-Do Han, So Yoon Kwon, So Hee Park, You-Bin Lee, Sang-Man Jin, Jae Hyeon Kim
Cardiovascular Diabetology.2022;[Epub] CrossRef - Cumulative Exposure to High γ-Glutamyl Transferase Level and Risk of Diabetes: A Nationwide Population-Based Study
Ji-Yeon Park, Kyungdo Han, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Mee Kyoung Kim, Seung-Hwan Lee
Endocrinology and Metabolism.2022; 37(2): 272. CrossRef - SGLT-2 inhibitors and GLP-1 receptor agonists in metabolic dysfunction-associated fatty liver disease
Jun Sung Moon, Jun Hwa Hong, Yong Jin Jung, Ele Ferrannini, Michael A. Nauck, Soo Lim
Trends in Endocrinology & Metabolism.2022; 33(6): 424. CrossRef - Plasma Aldo-Keto Reductase Family 1 Member B10 as a Biomarker Performs Well in the Diagnosis of Nonalcoholic Steatohepatitis and Fibrosis
Aron Park, Seung Joon Choi, Sungjin Park, Seong Min Kim, Hye Eun Lee, Minjae Joo, Kyoung Kon Kim, Doojin Kim, Dong Hae Chung, Jae Been Im, Jaehun Jung, Seung Kak Shin, Byung-Chul Oh, Cheolsoo Choi, Seungyoon Nam, Dae Ho Lee
International Journal of Molecular Sciences.2022; 23(9): 5035. CrossRef - Chinese Herbal Medicine for Type 2 Diabetes Mellitus With Nonalcoholic Fatty Liver Disease: A Systematic Review and Meta-Analysis
Sihan Peng, Lu Liu, Ziyan Xie, Xiyu Zhang, Chunguang Xie, Sha Ye, Xiangeng Zhang, Xiaoli Liang, Hongyan Wang, Ya Liu
Frontiers in Pharmacology.2022;[Epub] CrossRef - Non-alcoholic fatty liver disease and sarcopenia is associated with the risk of albuminuria independent of insulin resistance, and obesity
Eugene Han, Mi Kyung Kim, Seung-Soon Im, Byoung Kuk Jang, Hye Soon Kim
Journal of Diabetes and its Complications.2022; 36(8): 108253. CrossRef - Extra-Glycemic Effects of Anti-Diabetic Medications: Two Birds with One Stone?
Eun-Jung Rhee
Endocrinology and Metabolism.2022; 37(3): 415. CrossRef - Plasma Metabolomics and Machine Learning-Driven Novel Diagnostic Signature for Non-Alcoholic Steatohepatitis
Moongi Ji, Yunju Jo, Seung Joon Choi, Seong Min Kim, Kyoung Kon Kim, Byung-Chul Oh, Dongryeol Ryu, Man-Jeong Paik, Dae Ho Lee
Biomedicines.2022; 10(7): 1669. CrossRef - Association Between DPP4 Inhibitor Use and the Incidence of Cirrhosis, ESRD, and Some Cancers in Patients With Diabetes
Yewon Na, Soo Wan Kim, Ie Byung Park, Soo Jung Choi, Seungyoon Nam, Jaehun Jung, Dae Ho Lee
The Journal of Clinical Endocrinology & Metabolism.2022; 107(11): 3022. CrossRef - Nonalcoholic fatty liver disease is associated with early left ventricular diastolic dysfunction in patients with type 2 diabeteS
Walaa Sheba, Eman Morsy, Salah Altahan, Mona Ayaad, Sameh A. Lashen
Alexandria Journal of Medicine.2022; 58(1): 117. CrossRef - The association between changes in hepatic steatosis and hepatic fibrosis with cardiovascular outcomes and mortality in patients with New-Onset type 2 Diabetes: A nationwide cohort study
Jiyun Park, Gyuri Kim, Bong-Sung Kim, Kyung-Do Han, So Yoon Kwon, So Hee Park, You-Bin Lee, Sang-Man Jin, Jae Hyeon Kim
Diabetes Research and Clinical Practice.2022; 194: 110191. CrossRef - Advanced Liver Fibrosis Is Associated with Chronic Kidney Disease in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease (Diabetes Metab J 2022;46:630-9)
Ji Hye Huh
Diabetes & Metabolism Journal.2022; 46(6): 953. CrossRef - The association of fatty liver index and BARD score with all-cause and cause-specific mortality in patients with type 2 diabetes mellitus: a nationwide population-based study
Goh Eun Chung, Su-Min Jeong, Eun Ju Cho, Ji Won Yoon, Jeong-Ju Yoo, Yuri Cho, Kyu-na Lee, Dong Wook Shin, Yoon Jun Kim, Jung-Hwan Yoon, Kyungdo Han, Su Jong Yu
Cardiovascular Diabetology.2022;[Epub] CrossRef - Non-Albumin Proteinuria (NAP) as a Complementary Marker for Diabetic Kidney Disease (DKD)
Jaehyun Bae, Young Jun Won, Byung-Wan Lee
Life.2021; 11(3): 224. CrossRef - Diabetes Mellitus and Non-Alcoholic Fatty Liver Disease: Diagnosis and Treatment
Sook Jung Lee, Byung-Wan Lee
The Journal of Korean Diabetes.2021; 22(1): 38. CrossRef - Non-alcoholic fatty liver disease
Elizabeth E Powell, Vincent Wai-Sun Wong, Mary Rinella
The Lancet.2021; 397(10290): 2212. CrossRef - Allopurinol ameliorates high fructose diet induced hepatic steatosis in diabetic rats through modulation of lipid metabolism, inflammation, and ER stress pathway
In-Jin Cho, Da-Hee Oh, Jin Yoo, You-Cheol Hwang, Kyu Jeung Ahn, Ho-Yeon Chung, Soung Won Jeong, Ju-Young Moon, Sang-Ho Lee, Sung-Jig Lim, In-Kyung Jeong
Scientific Reports.2021;[Epub] CrossRef - Patient Management in Non-Alcoholic Fatty Liver Disease and Type 2 Diabetes Mellitus
A. E. Bagriy, A. D. Zubov, M. V. Khomenko, E. S. Mikhailichenko, E. A. Pylaeva, N. A. Khaustova, E. V. Bryukhovetskaya
Russian Journal of Gastroenterology, Hepatology, Coloproctology.2021; 31(2): 14. CrossRef - Liver Fibrosis Indices for the Prediction of Mortality in Korean Subjects: A 16-Year Prospective Cohort Study
Tae Jung Oh, Kyuho Kim, Jae Hoon Moon, Sung Hee Choi, Nam H Cho, Hak Chul Jang
Journal of the Endocrine Society.2021;[Epub] CrossRef - Reduced Rank Regression-Derived Dietary Patterns Related to the Fatty Liver Index and Associations with Type 2 Diabetes Mellitus among Ghanaian Populations under Transition: The RODAM Study
Tracy Bonsu Osei, Anne-Marieke van Dijk, Sjoerd Dingerink, Felix Patience Chilunga, Erik Beune, Karlijn Anna Catharina Meeks, Silver Bahendeka, Matthias Bernd Schulze, Charles Agyemang, Mary Nicolaou, Adriaan Georgius Holleboom, Ina Danquah
Nutrients.2021; 13(11): 3679. CrossRef - Efficacy and Safety of GLP-1 Receptor Agonists in Patients With Type 2 Diabetes Mellitus and Non-Alcoholic Fatty Liver Disease: A Systematic Review and Meta-Analysis
Yuan Zhu, Jiao Xu, Dong Zhang, Xingyu Mu, Yi Shi, Shangtao Chen, Zengxiang Wu, Shuangqing Li
Frontiers in Endocrinology.2021;[Epub] CrossRef - Liver fibrosis indices are related to diabetic peripheral neuropathy in individuals with type 2 diabetes
Kyuho Kim, Tae Jung Oh, Hyen Chung Cho, Yun Kyung Lee, Chang Ho Ahn, Bo Kyung Koo, Jae Hoon Moon, Sung Hee Choi, Hak Chul Jang
Scientific Reports.2021;[Epub] CrossRef - Evaluation of Grapefruit Juice in terms of Interleukin 18 Gene Expression in Rats with Fatty Liver and Healthy Rats
Simin Bahmanpoor, Noosha Zia-Jahromi
journal of ilam university of medical sciences.2021; 29(4): 74. CrossRef
- A combined extract containing Schisandra chinensis (SCE) reduced hepatic triglyceride accumulation in rats fed a high-sucrose diet
- Drug/Regimen
- Evogliptin, a Dipeptidyl Peptidase-4 Inhibitor, Attenuates Renal Fibrosis Caused by Unilateral Ureteral Obstruction in Mice
- Mi-Jin Kim, Na-young Kim, Yun-A Jung, Seunghyeong Lee, Gwon-Soo Jung, Jung-Guk Kim, In-Kyu Lee, Sungwoo Lee, Yeon-Kyung Choi, Keun-Gyu Park
- Diabetes Metab J. 2020;44(1):186-192. Published online October 31, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0271
- 5,660 View
- 97 Download
- 10 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Renal fibrosis is considered to be the final common outcome of chronic kidney disease. Dipeptidyl peptidase-4 (DPP-4) inhibitors have demonstrated protective effects against diabetic kidney disease. However, the anti-fibrotic effect of evogliptin, a DPP-4 inhibitor, has not been studied. Here, we report the beneficial effects of evogliptin on unilateral ureteral obstruction (UUO)-induced renal fibrosis in mice. Evogliptin attenuated UUO-induced renal atrophy and tubulointerstitial fibrosis. Immunohistochemistry and Western blotting demonstrated that evogliptin treatment inhibits pro-fibrotic gene expressions and extracellular matrix production.
In vitro findings showed that the beneficial effects of evogliptin on renal fibrosis are mediated by inhibition of the transforming growth factor-β/Smad3 signaling pathway. The present study demonstrates that evogliptin is protective against UUO-induced renal fibrosis, suggesting that its clinical applications could extend to the treatment of kidney disease of non-diabetic origin.-
Citations
Citations to this article as recorded by- Targeting cluster of differentiation 26 / dipeptidyl peptidase 4 (CD26/DPP4) in organ fibrosis
Birte Ohm, Isabelle Moneke, Wolfgang Jungraithmayr
British Journal of Pharmacology.2023; 180(22): 2846. CrossRef - Linagliptin ameliorates pulmonary fibrosis in systemic sclerosis mouse model via inhibition of endothelial-to-mesenchymal transition
Biwei Pei, Na Zhang, Tingting Pang, Gengyun Sun
Molecular and Cellular Biochemistry.2022; 477(4): 995. CrossRef - Association Between DPP4 Inhibitor Use and the Incidence of Cirrhosis, ESRD, and Some Cancers in Patients With Diabetes
Yewon Na, Soo Wan Kim, Ie Byung Park, Soo Jung Choi, Seungyoon Nam, Jaehun Jung, Dae Ho Lee
The Journal of Clinical Endocrinology & Metabolism.2022; 107(11): 3022. CrossRef - Evogliptin Directly Inhibits Inflammatory and Fibrotic Signaling in Isolated Liver Cells
Hye-Young Seo, So-Hee Lee, Eugene Han, Jae Seok Hwang, Sol Han, Mi Kyung Kim, Byoung Kuk Jang
International Journal of Molecular Sciences.2022; 23(19): 11636. CrossRef - Optimization and validation of a fluorogenic dipeptidyl peptidase 4 enzymatic assay in human plasma
Hyunyee Yoon, Su Hee Cho, Yu Rim Seo, Kyung-Sang Yu, Sung Sup Park, Moon Jung Song
Analytical Biochemistry.2021; 612: 113952. CrossRef - Use of Anti-Diabetic Agents in Non-Diabetic Kidney Disease: From Bench to Bedside
Sungjin Chung, Gheun-Ho Kim
Life.2021; 11(5): 389. CrossRef - Targeting Dermal Fibroblast Subtypes in Antifibrotic Therapy: Surface Marker as a Cellular Identity or a Functional Entity?
Xin Huang, Yimin Khoong, Chengyao Han, Dai Su, Hao Ma, Shuchen Gu, Qingfeng Li, Tao Zan
Frontiers in Physiology.2021;[Epub] CrossRef - Efficacy and safety of evogliptin treatment in patients with type 2 diabetes: A multicentre, active‐controlled, randomized, double‐blind study with open‐label extension (the EVERGREEN study)
Gyuri Kim, Soo Lim, Hyuk‐Sang Kwon, Ie B. Park, Kyu J. Ahn, Cheol‐Young Park, Su K. Kwon, Hye S. Kim, Seok W. Park, Sin G. Kim, Min K. Moon, Eun S. Kim, Choon H. Chung, Kang S. Park, Mikyung Kim, Dong J. Chung, Chang B. Lee, Tae H. Kim, Moon‐Kyu Lee
Diabetes, Obesity and Metabolism.2020; 22(9): 1527. CrossRef Effect of Switching from Linagliptin to Teneligliptin Dipeptidyl Peptidase-4 Inhibitors in Older Patients with Type 2 Diabetes Mellitus
Eugene Han, Minyoung Lee, Yong-ho Lee, Hye Soon Kim, Byung-wan Lee, Bong-Soo Cha, Eun Seok Kang
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 4113. CrossRef- Efficacy and safety of novel dipeptidyl-peptidase-4 inhibitor evogliptin in the management of type 2 diabetes mellitus: A meta-analysis
Deep Dutta, Saptarshi Bhattacharya, Aishwarya Krishnamurthy, LokeshKumar Sharma, Meha Sharma
Indian Journal of Endocrinology and Metabolism.2020; 24(5): 434. CrossRef
- Targeting cluster of differentiation 26 / dipeptidyl peptidase 4 (CD26/DPP4) in organ fibrosis
- Epidemiology
- Low-Normal Free Thyroxine Levels in Euthyroid Male Are Associated with Prediabetes
- Sung Woo Kim, Jae-Han Jeon, Jun Sung Moon, Eon Ju Jeon, Mi-Kyung Kim, In-Kyu Lee, Jung Beom Seo, Keun-Gyu Park
- Diabetes Metab J. 2019;43(5):718-726. Published online March 19, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0222
- 4,320 View
- 51 Download
- 2 Web of Science
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Abnormal thyroid function is associated with impaired glucose homeostasis. This study aimed to determine whether free thyroxine (FT4) influences the prevalence of prediabetes in euthyroid subjects using a cross-sectional survey derived from the Korea National Health and Nutrition Examination Survey, conducted between 2013 and 2015. We studied 2,399 male participants of >20 years of age who were euthyroid and non-diabetic. Prediabetic participants had lower FT4 concentrations than those without prediabetes, but their thyrotropin concentrations were similar. We stratified the population into tertiles according to FT4 concentration. After adjusting for multiple confounding factors, glycosylated hemoglobin (HbA1c) levels significantly decreased with increasing FT4 tertile, whereas fasting plasma glucose (FPG) levels were not associated with FT4 tertiles (HbA1c,
P <0.01 in T3 vs. T1; FPG,P =0.489 in T3 vs. T1). The prevalence of prediabetes was significantly higher in T1 (odds ratio, 1.426; 95% confidence interval, 1.126 to 1.806;P <0.01) than in T3. In conclusion, subjects with low-normal serum FT4 had high HbA1c and were more likely to have prediabetes. These results suggest that low FT4 concentration is a risk factor for prediabetes in male, even when thyroid function is within the normal range.
- Complications
- Gemigliptin Attenuates Renal Fibrosis Through Down-Regulation of the NLRP3 Inflammasome
- Jung Beom Seo, Yeon-Kyung Choi, Hye-In Woo, Yun-A Jung, Sungwoo Lee, Seunghyeong Lee, Mihyang Park, In-Kyu Lee, Gwon-Soo Jung, Keun-Gyu Park
- Diabetes Metab J. 2019;43(6):830-839. Published online March 5, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0181
- 5,416 View
- 128 Download
- 23 Web of Science
- 24 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The hypoglycemic drugs dipeptidyl peptidase-4 (DPP-4) inhibitors have proven protective effects on diabetic kidney disease, including renal fibrosis. Although NOD-like receptor protein 3 (NLRP3) inflammasome activation is known to play an important role in the progression of renal fibrosis, the impact of DPP-4 inhibition on NLRP3-mediated inflammation while ameliorating renal fibrosis has not been fully elucidated. Here, we report that the renoprotective effect of gemigliptin is associated with a reduction in NLRP3-mediated inflammation in a murine model of renal fibrosis.
Methods We examined the effects of gemigliptin on renal tubulointerstitial fibrosis induced in mice by unilateral ureteral obstruction (UUO). Using immunohistochemical and Western blot analysis, we quantitated components of the NLRP3 inflammasome in kidneys with and without gemigliptin treatment, and
in vitro in human kidney tubular epithelial human renal proximal tubule cells (HK-2) cells, we further analyzed the effect of gemigliptin on transforming growth factor-β (TGF-β)-stimulated production of profibrotic proteins.Results Immunohistological examination revealed that gemigliptin ameliorated UUO-induced tubular atrophy and renal fibrosis. Gemigliptin-treated kidneys showed a reduction in levels of NLRP3, apoptosis-associated speck-like protein containing a caspase recruitment domain (ASC), caspase-1, and interleukin-1β, which had all been markedly increased by UUO. In line with the
in vivo Conclusion The present study shows that activation of the NLRP3 inflammasome contributes to UUO-induced renal fibrosis and the renoprotective effect of gemigliptin is associated with attenuation of NLRP3 inflammasome activation.
-
Citations
Citations to this article as recorded by- Novel pharmacological interventions for diabetic kidney disease
Seng Kiong Tan, Jairo A. Pinzon-Cortes, Mark E. Cooper
Current Opinion in Nephrology & Hypertension.2024; 33(1): 13. CrossRef - Integrated analysis reveals crosstalk between pyroptosis and immune regulation in renal fibrosis
Fengxia Bai, Longchao Han, Jifeng Yang, Yuxiu Liu, Xiangmeng Li, Yaqin Wang, Ruijian Jiang, Zhaomu Zeng, Yan Gao, Haisong Zhang
Frontiers in Immunology.2024;[Epub] CrossRef - Di (2-ethylhexyl) phthalate and polystyrene microplastics co-exposure caused oxidative stress to activate NF-κB/NLRP3 pathway aggravated pyroptosis and inflammation in mouse kidney
Shanshan Li, Xuedie Gu, Muyue Zhang, Qihang Jiang, Tong Xu
Science of The Total Environment.2024; 926: 171817. CrossRef - Fluorofenidone attenuates renal fibrosis by inhibiting lysosomal cathepsin‑mediated NLRP3 inflammasome activation
Linfeng Zheng, Wenjuan Mei, Jing Zhou, Xin Wei, Zhijuan Huang, Xiaozhen Lin, Li Zhang, Wei Liu, Qian Wu, Jinhong Li, Yan Yan
Experimental and Therapeutic Medicine.2024;[Epub] CrossRef - HIF1α-BNIP3-mediated mitophagy protects against renal fibrosis by decreasing ROS and inhibiting activation of the NLRP3 inflammasome
Jialin Li, Qisheng Lin, Xinghua Shao, Shu Li, Xuying Zhu, Jingkui Wu, Shan Mou, Leyi Gu, Qin Wang, Minfang Zhang, Kaiqi Zhang, Jiayue Lu, Zhaohui Ni
Cell Death & Disease.2023;[Epub] CrossRef - Pyroptosis in renal inflammation and fibrosis: current knowledge and clinical significance
Ya Liu, Haibo Lei, Wenyou Zhang, Qichang Xing, Renzhu Liu, Shiwei Wu, Zheng Liu, Qingzi Yan, Wencan Li, Xiang Liu, Yixiang Hu
Cell Death & Disease.2023;[Epub] CrossRef - Tubular injury in diabetic kidney disease: molecular mechanisms and potential therapeutic perspectives
Yu Wang, Mingyue Jin, Chak Kwong Cheng, Qiang Li
Frontiers in Endocrinology.2023;[Epub] CrossRef - Hederagenin inhibits high glucose‐induced fibrosis in human renal cells by suppression of NLRP3 inflammasome activation through reducing cathepsin B expression
Guohua Yang, Wang Yang, Hairong Jiang, Qing Yi, Wei Ma
Chemical Biology & Drug Design.2023; 102(6): 1409. CrossRef - Obstructive nephropathy and molecular pathophysiology of renal interstitial fibrosis
Rikke Nørregaard, Henricus A. M. Mutsaers, Jørgen Frøkiær, Tae-Hwan Kwon
Physiological Reviews.2023; 103(4): 2847. CrossRef - Adenine model of chronic renal failure in rats to determine whether MCC950, an NLRP3 inflammasome inhibitor, is a renopreventive
Mahmoud S. Sabra, Fahmy K. Hemida, Essmat A. H. Allam
BMC Nephrology.2023;[Epub] CrossRef - Gut microbiota dysbiosis promotes age-related atrial fibrillation by lipopolysaccharide and glucose-induced activation of NLRP3-inflammasome
Yun Zhang, Song Zhang, Bolin Li, Yingchun Luo, Yongtai Gong, Xuexin Jin, Jiawei Zhang, Yun Zhou, Xiaozhen Zhuo, Zixi Wang, Xinbo Zhao, Xuejie Han, Yunlong Gao, Hui Yu, Desen Liang, Shiqi Zhao, Danghui Sun, Dingyu Wang, Wei Xu, Guangjin Qu, Wanlan Bo, Dan
Cardiovascular Research.2022; 118(3): 785. CrossRef - The NLRP3 inflammasome in fibrosis and aging: The known unknowns
Yanqing Liu, Xuezeng Xu, Wangrui Lei, Yuxuan Hou, Yan Zhang, Ran Tang, Zhi Yang, Ye Tian, Yanli Zhu, Changyu Wang, Chao Deng, Shaofei Zhang, Yang Yang
Ageing Research Reviews.2022; 79: 101638. CrossRef - Research progress of endothelial‐mesenchymal transition in diabetic kidney disease
Ying Chen, Hang Zou, Hongwei Lu, Hong Xiang, Shuhua Chen
Journal of Cellular and Molecular Medicine.2022; 26(12): 3313. CrossRef - Exploring the mechanism of Shendi Bushen capsule in anti-renal fibrosis using metabolomics theory and network analysis
Tianwei Meng, Hong Chang, Hongyu Meng
Molecular Omics.2022; 18(9): 873. CrossRef - Gemigliptin suppresses salivary dysfunction in streptozotocin-induced diabetic rats
Wan Seok Kang, Woo Kwon Jung, Su-Bin Park, Hyung Rae Kim, Junghyun Kim
Biomedicine & Pharmacotherapy.2021; 137: 111297. CrossRef - Long‐Term Dipeptidyl Peptidase 4 Inhibition Worsens Hypertension and Renal and Cardiac Abnormalities in Obese Spontaneously Hypertensive Heart Failure Rats
Edwin K. Jackson, Zaichuan Mi, Delbert G. Gillespie, Dongmei Cheng, Stevan P. Tofovic
Journal of the American Heart Association.2021;[Epub] CrossRef - Disulfiram inhibits inflammation and fibrosis in a rat unilateral ureteral obstruction model by inhibiting gasdermin D cleavage and pyroptosis
Yu Zhang, Ruicheng Zhang, Xiaohu Han
Inflammation Research.2021; 70(5): 543. CrossRef - Inflammasome as an Effective Platform for Fibrosis Therapy
Ting-Ting Chen, Feng Xiao, Nan Li, Shan Shan, Meng Qi, Zi-Ying Wang, Sheng-Nan Zhang, Wei Wei, Wu-Yi Sun
Journal of Inflammation Research.2021; Volume 14: 1575. CrossRef - Targeting Dermal Fibroblast Subtypes in Antifibrotic Therapy: Surface Marker as a Cellular Identity or a Functional Entity?
Xin Huang, Yimin Khoong, Chengyao Han, Dai Su, Hao Ma, Shuchen Gu, Qingfeng Li, Tao Zan
Frontiers in Physiology.2021;[Epub] CrossRef - Linagliptin Protects against Endotoxin-Induced Acute Kidney Injury in Rats by Decreasing Inflammatory Cytokines and Reactive Oxygen Species
Tsung-Jui Wu, Yi-Jen Hsieh, Chia-Wen Lu, Chung-Jen Lee, Bang-Gee Hsu
International Journal of Molecular Sciences.2021; 22(20): 11190. CrossRef - Psidium guajava Flavonoids Prevent NLRP3 Inflammasome Activation and Alleviate the Pancreatic Fibrosis in a Chronic Pancreatitis Mouse Model
Guixian Zhang, Liming Tang, Hongbin Liu, Dawei Liu, Manxue Wang, Jun Cai, Weijun Liu, Wei Nie, Yi Zhang, Xiaomeng Yu
The American Journal of Chinese Medicine.2021; 49(08): 2001. CrossRef - Effect and Regulation of the NLRP3 Inflammasome During Renal Fibrosis
Hong Zhang, Zhengchao Wang
Frontiers in Cell and Developmental Biology.2020;[Epub] CrossRef - Zhen-Wu-Tang Protects IgA Nephropathy in Rats by Regulating Exosomes to Inhibit NF-κB/NLRP3 Pathway
Honglian Li, Ruirui Lu, Yu Pang, Jicheng Li, Yiwen Cao, Hongxin Fu, Guoxing Fang, Qiuhe Chen, Bihao Liu, Junbiao Wu, Yuan Zhou, Jiuyao Zhou
Frontiers in Pharmacology.2020;[Epub] CrossRef - Protective effect of exogenous hydrogen sulfide on diaphragm muscle fibrosis in streptozotocin-induced diabetic rats
Rui Yang, Qiang Jia, Yan Li, Shomaila Mehmood
Experimental Biology and Medicine.2020; 245(14): 1280. CrossRef
- Novel pharmacological interventions for diabetic kidney disease
- Islet Studies and Transplantation
-
- Myricetin Protects Against High Glucose-Induced β-Cell Apoptosis by Attenuating Endoplasmic Reticulum Stress via Inactivation of Cyclin-Dependent Kinase 5
- Udayakumar Karunakaran, Suma Elumalai, Jun Sung Moon, Jae-Han Jeon, Nam Doo Kim, Keun-Gyu Park, Kyu Chang Won, Jaechan Leem, In-Kyu Lee
- Diabetes Metab J. 2019;43(2):192-205. Published online January 16, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0052
- 4,904 View
- 106 Download
- 33 Web of Science
- 32 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Chronic hyperglycemia has deleterious effects on pancreatic β-cell function and turnover. Recent studies support the view that cyclin-dependent kinase 5 (CDK5) plays a role in β-cell failure under hyperglycemic conditions. However, little is known about how CDK5 impair β-cell function. Myricetin, a natural flavonoid, has therapeutic potential for the treatment of type 2 diabetes mellitus. In this study, we examined the effect of myricetin on high glucose (HG)-induced β-cell apoptosis and explored the relationship between myricetin and CDK5.
Methods To address this question, we subjected INS-1 cells and isolated rat islets to HG conditions (30 mM) in the presence or absence of myricetin. Docking studies were conducted to validate the interaction between myricetin and CDK5. Gene expression and protein levels of endoplasmic reticulum (ER) stress markers were measured by real-time reverse transcription polymerase chain reaction and Western blot analysis.
Results Activation of CDK5 in response to HG coupled with the induction of ER stress via the down regulation of sarcoendoplasmic reticulum calcium ATPase 2b (
SERCA2b ) gene expression and reduced the nuclear accumulation of pancreatic duodenal homeobox 1 (PDX1) leads to β-cell apoptosis. Docking study predicts that myricetin inhibit CDK5 activation by direct binding in the ATP-binding pocket. Myricetin counteracted the decrease in the levels of PDX1 and SERCA2b by HG. Moreover, myricetin attenuated HG-induced apoptosis in INS-1 cells and rat islets and reduce the mitochondrial dysfunction by decreasing reactive oxygen species production and mitochondrial membrane potential (Δψm) loss.Conclusion Myricetin protects the β-cells against HG-induced apoptosis by inhibiting ER stress, possibly through inactivation of CDK5 and consequent upregulation of PDX1 and SERCA2b.
-
Citations
Citations to this article as recorded by- Profiling of secondary metabolite and evaluation of anti-diabetic potency of Crotalaria quinquefolia (L): In-vitro, in-vivo, and in-silico approaches
Nazmun Nahar, Md. Nazmul Hasan Zilani, Partha Biswas, Md. Morsaline Billah, Shabana Bibi, Norah A. Albekairi, Abdulrahman Alshammari, Md. Nazmul Hasan
Saudi Pharmaceutical Journal.2024; 32(1): 101887. CrossRef - Mitochondrial aldehyde dehydrogenase-2 coordinates the hydrogen sulfide - AMPK axis to attenuate high glucose-induced pancreatic β-cell dysfunction by glutathione antioxidant system
Udayakumar Karunakaran, Suma Elumalai, Seung Min Chung, Kathrin Maedler, Kyu Chang Won, Jun Sung Moon
Redox Biology.2024; 69: 102994. CrossRef - Network-based identification and mechanism exploration of active ingredients against Alzheimer’s disease via targeting endoplasmic reticulum stress from traditional chinese medicine
Zhao Dai, Tian Hu, Junwen Wei, Xue Wang, Chuipu Cai, Yong Gu, Yunhui Hu, Wenjia Wang, Qihui Wu, Jiansong Fang
Computational and Structural Biotechnology Journal.2024; 23: 506. CrossRef - Myricetin as a Promising Flavonoid with Multitargeted Biological Activity
A.S. Chiriapkin
Juvenis Scientia.2024; 10(1): 5. CrossRef - Naturally occurring small molecules with dual effect upon inflammatory signaling pathways and endoplasmic reticulum stress response
Daniela Correia da Silva, Patrícia Valentão, David M. Pereira
Journal of Physiology and Biochemistry.2024;[Epub] CrossRef - Omnifarious fruit polyphenols: an omnipotent strategy to prevent and intervene diabetes and related complication?
Yao Chen, Xuejiao Qie, Wei Quan, Maomao Zeng, Fang Qin, Jie Chen, Benu Adhikari, Zhiyong He
Critical Reviews in Food Science and Nutrition.2023; 63(20): 4288. CrossRef - Regulation of reactive oxygen species by phytochemicals for the management of cancer and diabetes
Heui Min Lim, See-Hyoung Park
Critical Reviews in Food Science and Nutrition.2023; 63(22): 5911. CrossRef - Bioactive compounds from Polygonatum genus as anti-diabetic agents with future perspectives
Yan Shi, Dun Si, Donghong Chen, Xinfeng Zhang, Zhigang Han, Qiang Yu, Jingjing Liu, Jinping Si
Food Chemistry.2023; 408: 135183. CrossRef - Venom Peptides, Polyphenols and Alkaloids: Are They the Next Antidiabetics That Will Preserve β-Cell Mass and Function in Type 2 Diabetes?
Michele Lodato, Valérie Plaisance, Valérie Pawlowski, Maxime Kwapich, Alexandre Barras, Emeline Buissart, Stéphane Dalle, Sabine Szunerits, Jérôme Vicogne, Rabah Boukherroub, Amar Abderrahmani
Cells.2023; 12(6): 940. CrossRef - TFP5 attenuates cyclin‐dependent kinase 5‐mediated islet β‐cell damage in diabetes
Shunyao Liu, Bo Li, Danna Ma, Yuejia Tao, Jiang Song, Li Bao, Guoqing Zhang, Hongyan Luo, Shilu Cao, Jing E, Yali Zheng
Chemical Biology & Drug Design.2023; 102(1): 76. CrossRef - Antiviral and Possible Prophylactic Significance of Myricetin for COVID-19
Pawan K. Agrawal, Chandan Agrawal, Gerald Blunden
Natural Product Communications.2023; 18(4): 1934578X2311662. CrossRef - In Vitro and In Silico Protocols for the Assessment of Anti-Tick Compounds from Pinus roxburghii against Rhipicephalus (Boophilus) microplus Ticks
Sana Ayub, Nosheen Malak, Raquel Cossío-Bayúgar, Nasreen Nasreen, Afshan Khan, Sadaf Niaz, Adil Khan, Abdallah D. Alanazi, Mourad Ben Said
Animals.2023; 13(8): 1388. CrossRef - Protective Effect of Myricetin Against Experimentally Induced Torsion in Rats
M. Tatar, Z. Polat, J. Öner, H. Öner
Biology Bulletin.2023; 50(6): 1338. CrossRef - The pharmacological mechanism of Abelmoschus manihot in the treatment of chronic kidney disease
Cuiting Wei, Chao Wang, Run Li, Yunfeng Bai, Xue Wang, Qingyun Fang, Xiangmei Chen, Ping Li
Heliyon.2023; 9(11): e22017. CrossRef - Natural Polyphenols as SERCA Activators: Role in the Endoplasmic Reticulum Stress-Related Diseases
Jana Viskupicova, Petronela Rezbarikova
Molecules.2022; 27(16): 5095. CrossRef - Research progress on the mechanism of beta-cell apoptosis in type 2 diabetes mellitus
SuFang You, JingYi Zheng, YuPing Chen, HuiBin Huang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Myricetin inhibits pseudorabies virus infection through direct inactivation and activating host antiviral defense
Huaiyue Hu, Zhiqiang Hu, Yingying Zhang, Hongping Wan, Zhongqiong Yin, Lixia Li, Xiaoxia Liang, Xinghong Zhao, Lizi Yin, Gang Ye, Yuan-Feng Zou, Huaqiao Tang, Renyong Jia, Yaqin Chen, Hao Zhou, Xu Song
Frontiers in Microbiology.2022;[Epub] CrossRef - Effects of myricetin against cadmium-induced neurotoxicity in PC12 cells
Azadeh Aminzadeh, Ayda Salarinejad
Toxicology Research.2021; 10(1): 84. CrossRef - Pioglitazone-induced AMPK-Glutaminase-1 prevents high glucose-induced pancreatic β-cell dysfunction by glutathione antioxidant system
Udayakumar Karunakaran, Suma Elumalai, Jun Sung Moon, Kyu Chang Won
Redox Biology.2021; 45: 102029. CrossRef - Chlorogenic acid and β-glucan from highland barley grain ameliorate β-cell dysfunction via inhibiting apoptosis and improving cell proliferation
Ze-Hua Liu, Bo Li
Food & Function.2021; 12(20): 10040. CrossRef - The cyclin dependent kinase inhibitor Roscovitine prevents diet-induced metabolic disruption in obese mice
Nabil Rabhi, Kathleen Desevin, Briana Noel Cortez, Ryan Hekman, Jean Z. Lin, Andrew Emili, Stephen R. Farmer
Scientific Reports.2021;[Epub] CrossRef - AdipoRon promotes diabetic fracture repair through endochondral ossification-based bone repair by enhancing survival and differentiation of chondrocytes
Zhongyi Wang, Jinxin Tang, Ying Li, Yu Wang, Yanyang Guo, Qisheng Tu, Jake Chen, Chen Wang
Experimental Cell Research.2020; 387(2): 111757. CrossRef - A kinase of many talents: non-neuronal functions of CDK5 in development and disease
Samanta Sharma, Piotr Sicinski
Open Biology.2020; 10(1): 190287. CrossRef - Mitochondrial dysfunction in the fetoplacental unit in gestational diabetes mellitus
Luis Sobrevia, Paola Valero, Adriana Grismaldo, Roberto Villalobos-Labra, Fabián Pardo, Mario Subiabre, Gael Armstrong, Fernando Toledo, Sofía Vega, Marcelo Cornejo, Gonzalo Fuentes, Reinaldo Marín
Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.2020; 1866(12): 165948. CrossRef - Myricetin bioactive effects: moving from preclinical evidence to potential clinical applications
Yasaman Taheri, Hafiz Ansar Rasul Suleria, Natália Martins, Oksana Sytar, Ahmet Beyatli, Balakyz Yeskaliyeva, Gulnaz Seitimova, Bahare Salehi, Prabhakar Semwal, Sakshi Painuli, Anuj Kumar, Elena Azzini, Miquel Martorell, William N. Setzer, Alfred Maroyi,
BMC Complementary Medicine and Therapies.2020;[Epub] CrossRef - Current Pharmacological Trends on Myricetin
Gudiya Gupta, Mohd Aftab Siddiqui, Mohd Muazzam Khan, Mohd Ajmal, Rabiya Ahsan, Md Azizur Rahaman, Md Afroz Ahmad, Md Arshad, Mohammad Khushtar
Drug Research.2020;[Epub] CrossRef - Silencing cyclophilin A improves insulin secretion, reduces cell apoptosis, and alleviates inflammation as well as oxidant stress in high glucose-induced pancreatic β-cells via MAPK/NF-kb signaling pathway
Tangying Li, Huibiao Quan, Huachuan Zhang, Leweihua Lin, Qianying Ou, Kaining Chen
Bioengineered.2020; 11(1): 1047. CrossRef - Endoplasmic reticulum stress contributes to NMDA-induced pancreatic β-cell dysfunction in a CHOP-dependent manner
Xiao-Ting Huang, Wei Liu, Yong Zhou, Mei Sun, Chen-Chen Sun, Chen-Yu Zhang, Si-Yuan Tang
Life Sciences.2019; 232: 116612. CrossRef - Dapagliflozin rescues endoplasmic reticulum stress-mediated cell death
Ryo Shibusawa, Eijiro Yamada, Shuichi Okada, Yasuyo Nakajima, Claire C. Bastie, Akito Maeshima, Kyoichi Kaira, Masanobu Yamada
Scientific Reports.2019;[Epub] CrossRef - Myricetin prevents thapsigargin-induced CDK5-P66Shc signalosome mediated pancreatic β-cell dysfunction
Udayakumar Karunakaran, Ji Eun Lee, Suma Elumalai, Jun Sung Moon, Kyu Chang Won
Free Radical Biology and Medicine.2019; 141: 59. CrossRef - CDK5: Key Regulator of Apoptosis and Cell Survival
Rabih Roufayel, Nimer Murshid
Biomedicines.2019; 7(4): 88. CrossRef - Oral DhHP-6 for the Treatment of Type 2 Diabetes Mellitus
Kai Wang, Yu Su, Yuting Liang, Yanhui Song, Liping Wang
International Journal of Molecular Sciences.2019; 20(6): 1517. CrossRef
- Profiling of secondary metabolite and evaluation of anti-diabetic potency of Crotalaria quinquefolia (L): In-vitro, in-vivo, and in-silico approaches
- Response: Serum Levels of PCSK9 Are Associated with Coronary Angiographic Severity in Patients with Acute Coronary Syndrome (
Diabetes Metab J 2018;42:207-14) - Sung Woo Kim, Keun-Gyu Park
- Diabetes Metab J. 2018;42(4):350-352. Published online August 21, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0138
- 3,661 View
- 38 Download
- 4 Web of Science
- 4 Crossref
-
 PDF
PDF PubReader
PubReader -
Citations
Citations to this article as recorded by- Plasma Levels of Proprotein Convertase Subtilisin/Kexin Type 9 Are Inversely Associated with N-Terminal Pro B-Type Natriuretic Peptide in Older Men and Women
Francesco Spannella, Federico Giulietti, Roberta Galeazzi, Anna Passarelli, Serena Re, Chiara Di Pentima, Massimiliano Allevi, Paolo Magni, Riccardo Sarzani
Biomedicines.2022; 10(8): 1961. CrossRef - PCSK9: Associated with cardiac diseases and their risk factors?
Yanan Guo, Binjie Yan, Shi Tai, Shenghua Zhou, Xi-Long Zheng
Archives of Biochemistry and Biophysics.2021; 704: 108717. CrossRef - Gut Lactobacillus Level Is a Predictive Marker for Coronary Atherosclerotic Lesions Progress and Prognosis in Patients With Acute Coronary Syndrome
Jing Gao, Jie Wang, Li-Li Zhao, Ting-Ting Yao, Yang Chen, Jing Ma, Xu Zhang, Jing-Xian Wang, Yuan Wang, Zhuang Cui, Yin Liu
Frontiers in Cellular and Infection Microbiology.2021;[Epub] CrossRef - Butein Synergizes with Statin to Upregulate Low-Density Lipoprotein Receptor ThroughHNF1α-Mediated PCSK9 Inhibition in HepG2 Cells
Jin-Taek Hwang, Hyo Jin Kim, Hyo-Kyoung Choi, Jae-Ho Park, Sangwon Chung, Min-Yu Chung
Journal of Medicinal Food.2020; 23(10): 1102. CrossRef
- Plasma Levels of Proprotein Convertase Subtilisin/Kexin Type 9 Are Inversely Associated with N-Terminal Pro B-Type Natriuretic Peptide in Older Men and Women
- Complications
- Serum Levels of PCSK9 Are Associated with Coronary Angiographic Severity in Patients with Acute Coronary Syndrome
- Kwi-Hyun Bae, Sung Woo Kim, Yeon-Kyung Choi, Jung Beom Seo, Namkyun Kim, Chang-Yeon Kim, Won Kee Lee, Sungwoo Lee, Jung Guk Kim, In-Kyu Lee, Jang Hoon Lee, Keun-Gyu Park
- Diabetes Metab J. 2018;42(3):207-214. Published online May 2, 2018
- DOI: https://doi.org/10.4093/dmj.2017.0081
- 4,930 View
- 54 Download
- 25 Web of Science
- 23 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Proprotein convertase subtilisin/kexin type 9 (PCSK9) is a circulating protein that promotes degradation of the low density lipoprotein receptor. PCSK9 has emerged as a target for lipid-lowering therapy, but the predictive value of the serum level of PCSK9 for the severity of coronary disease is largely unknown.
Methods From December 2009 to July 2012, 121 individuals who underwent coronary angiography (CAG) because of clinically suspected acute coronary syndrome were enrolled in this study. Serum levels of PCSK9 and metabolic parameters were measured. SYNTAX (SYNergy between percutaneous coronary intervention with [paclitaxel-eluting] TAXUS stent and cardiac surgery) and GRACE (Global Registry of Acute Coronary Events) scores were calculated.
Results Individuals with CAG lesions (
n =100) had significantly higher levels of PCSK9 than those without lesions (n =21). The study population was stratified into three groups according to serum levels of PCSK9. The odds radio for occurrence of one or more CAG lesions was significantly higher in the group with the highest level of PCSK9 (odds ratio, 7.468;P =0.011) than in the group with the lowest level of PCSK9. Serum PCSK9 was positively associated with the number of involved coronary arteries. Multivariable linear regression indicated that levels of PCSK9 were positively correlated with GRACE risk scores and SYNTAX scores.Conclusion Serum PCSK9 concentrations are higher in patients with coronary artery lesions, and are associated with SYNTAX and GRACE scores, suggesting that PCSK9 is a potential biomarker of the severity of coronary artery disease.
-
Citations
Citations to this article as recorded by- Clinical Significance of PCSK9 and Soluble P-selectin in Predicting Major Adverse Cardiovascular Events After Primary Percutaneous Coronary Intervention in Patients with Acute Coronary Syndrome
Yao Yao, Qining Qiu, Xiaoye Li, Zi Wang, Shikun Xu, Qianzhou Lv
Cardiovascular Innovations and Applications.2024;[Epub] CrossRef - Stratification in Heterozygous Familial Hypercholesterolemia: Imaging, Biomarkers, and Genetic Testing
Pablo Corral, Carlos A. Aguilar Salinas, María Gabriela Matta, Valeria Zago, Laura Schreier
Current Atherosclerosis Reports.2023; 25(12): 899. CrossRef - Relationship of sortilin and proprotein convertase subtilisin/kexin type 9 in blood serum with the severity of carotid and coronary atherosclerosis in hypertensive patients
Yu. Yu. Vukolova, I. V. Gubareva
Russian Journal of Cardiology.2022; 27(2S): 4903. CrossRef - PCSK9 Inhibition could be Effective for Acute Myocardial Infarction
Baris Gencer, François Mach
Current Medicinal Chemistry.2022; 29(6): 1016. CrossRef - Peri-event plasma PCSK9 and hsCRP after an acute myocardial infarction correlate with early deterioration of left ventricular ejection fraction: a cohort study
Lina S. Silva-Bermúdez, Andrea Vargas-Villanueva, Carlos A. Sánchez-Vallejo, Ana C. Palacio, Andrés F. Buitrago, Carlos O. Mendivil
Lipids in Health and Disease.2022;[Epub] CrossRef - Plasma Levels of Proprotein Convertase Subtilisin/Kexin Type 9 Are Inversely Associated with N-Terminal Pro B-Type Natriuretic Peptide in Older Men and Women
Francesco Spannella, Federico Giulietti, Roberta Galeazzi, Anna Passarelli, Serena Re, Chiara Di Pentima, Massimiliano Allevi, Paolo Magni, Riccardo Sarzani
Biomedicines.2022; 10(8): 1961. CrossRef - Sex difference in circulating PCSK9 and its clinical implications
Fang Jia, Si-Fan Fei, De-Bing Tong, Cong Xue, Jian-Jun Li
Frontiers in Pharmacology.2022;[Epub] CrossRef - Physiology and role of PCSK9 in vascular disease: Potential impact of localized PCSK9 in vascular wall
Yanan Guo, Binjie Yan, Yu Gui, Zhihan Tang, Shi Tai, Shenghua Zhou, Xi‐Long Zheng
Journal of Cellular Physiology.2021; 236(4): 2333. CrossRef - PCSK9 levels do not predict severity and recurrence of cardiovascular events in patients with acute myocardial infarction
Marianne Zeller, Gilles Lambert, Michel Farnier, Maud Maza, Brice Nativel, Luc Rochette, Catherine Vergely, Yves Cottin
Nutrition, Metabolism and Cardiovascular Diseases.2021; 31(3): 880. CrossRef - Pcsk9 is associated with severity of coronary artery lesions in male patients with premature myocardial infarction
Jing Gao, Ya-Nan Yang, Zhuang Cui, Si-Yuan Feng, Jing Ma, Chang-Ping Li, Yin Liu
Lipids in Health and Disease.2021;[Epub] CrossRef - Circulating Biomarkers for Cardiovascular Disease Risk Prediction in Patients With Cardiovascular Disease
Yuen-Kwun Wong, Hung-Fat Tse
Frontiers in Cardiovascular Medicine.2021;[Epub] CrossRef - Association Between Circulating Proprotein Convertase Subtilisin/Kexin Type 9 Concentrations and Cardiovascular Events in Cardiovascular Disease: A Systemic Review and Meta-Analysis
Jiahui Liu, Fangfang Fan, Xingyu Luo, Wenjun Ji, Yaokun Liu, Yan Zhang, Bo Zheng
Frontiers in Cardiovascular Medicine.2021;[Epub] CrossRef - PCSK9 in acute coronary syndrome: analysis of associations with clinical and laboratory characteristics
Yu. A. Drenina, K. Yu. Nikolaev
Cardiovascular Therapy and Prevention.2020; 19(4): 2484. CrossRef - Relation of Proprotein Convertase Subtilisin/Kexin Type 9 to Cardiovascular Outcomes in Patients Undergoing Percutaneous Coronary Intervention
Ik Jun Choi, Sungmin Lim, Dongjae Lee, Won Jik Lee, Kwan Yong Lee, Mi-Jeong Kim, Doo Soo Jeon
The American Journal of Cardiology.2020; 133: 54. CrossRef - A Narrative Review and Expert Panel Recommendations on Dyslipidaemia Management After Acute Coronary Syndrome in Countries Outside Western Europe and North America
Ashraf Reda, Wael Almahmeed, Idit Dobrecky-Mery, Po-Hsun Huang, Ursulo Juarez-Herrera, Naresh Ranjith, Tobias Sayre, Miguel Urina-Triana
Advances in Therapy.2020; 37(5): 1754. CrossRef - PCSK9 concentrations in different stages of subclinical atherosclerosis and their relationship with inflammation
Štefan Tóth, Peter Olexa, Zdenka Hertelyová, Peter Štefanič, Ivan Kopolovets, Peter Berek, Vladimir Filip, Ryan Chakravarty, Monika Široká, Daniel Pella
Open Chemistry.2020; 18(1): 1011. CrossRef - Association of serum proprotein convertase subtilisin/kexin type 9 with early atherosclerosis in newly diagnosed type 2 diabetes mellitus
Wen Guo, Yingyun Gong, Jie Li, Pei Qin, Jing Lu, Xiaona Li, Wenfang Zhu, Nianzhen Xu, Hongwen Zhou, Qun Zhang
Nutrition, Metabolism and Cardiovascular Diseases.2019; 29(8): 815. CrossRef - PCSK9 and atherosclerosis burden in the coronary arteries of patients undergoing coronary angiography
Yunes Panahi, Mohsen Sadeghi Ghahrodi, Mohsen Jamshir, Mohammad Amin Safarpour, Vanessa Bianconi, Matteo Pirro, Maryam Moshkani Farahani, Amirhossein Sahebkar
Clinical Biochemistry.2019; 74: 12. CrossRef - Association of PCSK9 plasma levels with metabolic patterns and coronary atherosclerosis in patients with stable angina
Chiara Caselli, Serena Del Turco, Rosetta Ragusa, Valentina Lorenzoni, Michiel De Graaf, Giuseppina Basta, Arthur Scholte, Raffaele De Caterina, Danilo Neglia
Cardiovascular Diabetology.2019;[Epub] CrossRef - PCSK9 inhibition and inflammation: A narrative review
Massimiliano Ruscica, Lale Tokgözoğlu, Alberto Corsini, Cesare R. Sirtori
Atherosclerosis.2019; 288: 146. CrossRef - Letter: Serum Levels of PCSK9 Are Associated with Coronary Angiographic Severity in Patients with Acute Coronary Syndrome (Diabetes Metab J 2018;42:207-14)
Jin Hwa Kim
Diabetes & Metabolism Journal.2018; 42(4): 348. CrossRef - Response: Serum Levels of PCSK9 Are Associated with Coronary Angiographic Severity in Patients with Acute Coronary Syndrome (Diabetes Metab J 2018;42:207-14)
Sung Woo Kim, Keun-Gyu Park
Diabetes & Metabolism Journal.2018; 42(4): 350. CrossRef - Serum PCSK9 levels, but not PCSK9 polymorphisms, are associated with CAD risk and lipid profiles in southern Chinese Han population
Gaojun Cai, Lei Yu, Zhiying Huang, Li Li, Xingli Fu
Lipids in Health and Disease.2018;[Epub] CrossRef
- Clinical Significance of PCSK9 and Soluble P-selectin in Predicting Major Adverse Cardiovascular Events After Primary Percutaneous Coronary Intervention in Patients with Acute Coronary Syndrome
- Complications
- Renoprotective Effect of Gemigliptin, a Dipeptidyl Peptidase-4 Inhibitor, in Streptozotocin-Induced Type 1 Diabetic Mice
- Gwon-Soo Jung, Jae-Han Jeon, Mi Sun Choe, Sung-Woo Kim, In-Kyu Lee, Mi-Kyung Kim, Keun-Gyu Park
- Diabetes Metab J. 2016;40(3):211-221. Published online March 31, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.3.211
- 6,345 View
- 53 Download
- 22 Web of Science
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Dipeptidyl peptidase-4 (DPP-4) inhibitors are widely used in the treatment of patients with type 2 diabetes and have proven protective effects on diabetic kidney disease (DKD). Whether DPP-4 inhibitors have renoprotective effects on insulin-deficient type 1 diabetes has not been comprehensively examined. The aim of this study was to determine whether gemigliptin, a new DPP-4 inhibitor, has renoprotective effects in streptozotocin (STZ)-induced type 1 diabetic mice.
Methods Diabetes was induced by intraperitoneal administration of a single dose of STZ. Mice with diabetes were treated without or with gemigliptin (300 mg/kg) for 8 weeks. Morphological changes of the glomerular basement membrane (GBM) were observed by electron microscopy and periodic-acid Schiff staining. In addition, we measured blood glucose and urinary albumin excretion and evaluated fibrotic markers using immunohistochemical staining, quantitative reverse transcription polymerase chain reaction analysis, and Western blot analysis.
Results Gemigliptin did not reduce the blood glucose levels of STZ-treated mice. In gemigliptin-treated mice with STZ, a significant reduction in urinary albumin excretion and GBM thickness was observed. Immunohistological examination revealed that gemigliptin attenuated renal fibrosis induced by STZ and decreased extracellular matrix protein levels, including those of type I collagen and fibronectin, and Smad3 phosphorylation. In cultured rat renal cells, gemigliptin inhibited transforming growth factor β-stimulated type I collagen and fibronectin mRNA and protein levels via down-regulation of Smad3 phosphorylation.
Conclusion Our data demonstrate that gemigliptin has renoprotective effects on DKD, regardless of its glucose-lowering effect, suggesting that it could be used to prevent DKD, including in patients with type 1 diabetes.
-
Citations
Citations to this article as recorded by- Diabetic fibrosis
Izabela Tuleta, Nikolaos G. Frangogiannis
Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.2021; 1867(4): 166044. CrossRef - Protective roles of thymoquinone and vildagliptin in manganese-induced nephrotoxicity in adult albino rats
Heba El-Sayed Mostafa, Eman Ahmed Alaa El-Din, Dalia Abdallah El-Shafei, Nehal S. Abouhashem, Aisha Abdallah Abouhashem
Environmental Science and Pollution Research.2021; 28(24): 31174. CrossRef - Evogliptin, a Dipeptidyl Peptidase-4 Inhibitor, Attenuates Renal Fibrosis Caused by Unilateral Ureteral Obstruction in Mice
Mi-Jin Kim, Na-young Kim, Yun-A Jung, Seunghyeong Lee, Gwon-Soo Jung, Jung-Guk Kim, In-Kyu Lee, Sungwoo Lee, Yeon-Kyung Choi, Keun-Gyu Park
Diabetes & Metabolism Journal.2020; 44(1): 186. CrossRef - Gemigliptin Attenuates Renal Fibrosis Through Down-Regulation of the NLRP3 Inflammasome
Jung Beom Seo, Yeon-Kyung Choi, Hye-In Woo, Yun-A Jung, Sungwoo Lee, Seunghyeong Lee, Mihyang Park, In-Kyu Lee, Gwon-Soo Jung, Keun-Gyu Park
Diabetes & Metabolism Journal.2019; 43(6): 830. CrossRef - Recent advances in the pathogenesis of microvascular complications in diabetes
Sungmi Park, Hyeon-Ji Kang, Jae-Han Jeon, Min-Ji Kim, In-Kyu Lee
Archives of Pharmacal Research.2019; 42(3): 252. CrossRef - Diabetic nephropathy: An update on pathogenesis and drug development
Vikram Rao A/L B Vasanth Rao, Sean Hong Tan, Mayuren Candasamy, Subrat Kumar Bhattamisra
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(1): 754. CrossRef - Mechanisms and pathways of anti‐inflammatory activity of DPP‐4 inhibitors in cardiovascular and renal protection
Katarina Tomovic, Jelena Lazarevic, Gordana Kocic, Marina Deljanin‐Ilic, Marko Anderluh, Andrija Smelcerovic
Medicinal Research Reviews.2019; 39(1): 404. CrossRef - Effects of Dipeptidyl Peptidase-4 Inhibitors on Renal Outcomes in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis
Jae Hyun Bae, Sunhee Kim, Eun-Gee Park, Sin Gon Kim, Seokyung Hahn, Nam Hoon Kim
Endocrinology and Metabolism.2019; 34(1): 80. CrossRef - The emerging role of novel antihyperglycemic agents in the treatment of heart failure and diabetes: A focus on cardiorenal outcomes
Kelly R. McHugh, Adam D. DeVore, Robert J. Mentz, Daniel Edmonston, Jennifer B. Green, Adrian F. Hernandez
Clinical Cardiology.2018; 41(9): 1259. CrossRef - Acute Kidney Injury and Progression of Diabetic Kidney Disease
Samuel Mon-Wei Yu, Joseph V. Bonventre
Advances in Chronic Kidney Disease.2018; 25(2): 166. CrossRef - Recombinant human GLP-1(rhGLP-1) alleviating renal tubulointestitial injury in diabetic STZ-induced rats
Weiqin Yin, Shiqing Xu, Zai Wang, Honglin Liu, Liang Peng, Qing Fang, Tingting Deng, Wenjian Zhang, Jinning Lou
Biochemical and Biophysical Research Communications.2018; 495(1): 793. CrossRef - Chronic inhalation of e-cigarette vapor containing nicotine disrupts airway barrier function and induces systemic inflammation and multiorgan fibrosis in mice
Laura E. Crotty Alexander, Christopher A. Drummond, Mark Hepokoski, Denzil Mathew, Alex Moshensky, Andrew Willeford, Soumita Das, Prabhleen Singh, Zach Yong, Jasmine H. Lee, Kevin Vega, Ashley Du, John Shin, Christian Javier, Jiang Tian, Joan Heller Brown
American Journal of Physiology-Regulatory, Integrative and Comparative Physiology.2018; 314(6): R834. CrossRef - Renoprotective effect of fucoidan from Acaudina molpadioides in streptozotocin/high fat diet-induced type 2 diabetic mice
Shiwei Hu, Jinhui Wang, Jingfeng Wang, Shijie Li, Wei Jiang, Yu Liu
Journal of Functional Foods.2017; 31: 123. CrossRef - Dipeptidyl peptidase-4 inhibition and renoprotection
Yuta Takagaki, Daisuke Koya, Keizo Kanasaki
Current Opinion in Nephrology and Hypertension.2017; 26(1): 56. CrossRef - Treatment of diabetic kidney disease: current and future targets
Mi-Kyung Kim
The Korean Journal of Internal Medicine.2017; 32(4): 622. CrossRef - Pharmacological Treatment in Diabetes Mellitus Type 1 – Insulin and What Else?
Ewa Otto-Buczkowska, Natalia Jainta
International Journal of Endocrinology and Metabolism.2017;[Epub] CrossRef - GLP-1 and the kidney: from physiology to pharmacology and outcomes in diabetes
Marcel H. A. Muskiet, Lennart Tonneijck, Mark M. Smits, Michaël J.B. van Baar, Mark H. H. Kramer, Ewout J. Hoorn, Jaap A. Joles, Daniël H. van Raalte
Nature Reviews Nephrology.2017; 13(10): 605. CrossRef - Efficacy, safety and albuminuria‐reducing effect of gemigliptin in Korean type 2 diabetes patients with moderate to severe renal impairment: A 12‐week, double‐blind randomized study (the GUARD Study)
Sun A. Yoon, Byoung G. Han, Sung G. Kim, Sang Y. Han, Young I. Jo, Kyung H. Jeong, Kook H. Oh, Hyeong C. Park, Sun H. Park, Shin W. Kang, Ki R. Na, Sun W. Kang, Nam H. Kim, Young H. Jang, Seong H. Shin, Dae R. Cha
Diabetes, Obesity and Metabolism.2017; 19(4): 590. CrossRef - Sodium butyrate has context-dependent actions on dipeptidyl peptidase-4 and other metabolic parameters
Eun-Sol Lee, Dong-Sung Lee, Prakash Raj Pandeya, Youn-Chul Kim, Dae-Gil Kang, Ho-Sub Lee, Byung-Chul Oh, Dae Ho Lee
The Korean Journal of Physiology & Pharmacology.2017; 21(5): 519. CrossRef - Lobeglitazone, a Novel Peroxisome Proliferator-Activated Receptor γ Agonist, Attenuates Renal Fibrosis Caused by Unilateral Ureteral Obstruction in Mice
Kwi-Hyun Bae, Jung Beom Seo, Yun-A Jung, Hye-Young Seo, Sun Hee Kang, Hui-Jeon Jeon, Jae Man Lee, Sungwoo Lee, Jung-Guk Kim, In-Kyu Lee, Gwon-Soo Jung, Keun-Gyu Park
Endocrinology and Metabolism.2017; 32(1): 115. CrossRef - Gemigliptin: An Update of Its Clinical Use in the Management of Type 2 Diabetes Mellitus
Sung-Ho Kim, Jung-Hwa Yoo, Woo Je Lee, Cheol-Young Park
Diabetes & Metabolism Journal.2016; 40(5): 339. CrossRef - Risk assessment and management of post-transplant diabetes mellitus
Eugene Han, Myoung Soo Kim, Yu Seun Kim, Eun Seok Kang
Metabolism.2016; 65(10): 1559. CrossRef
- Diabetic fibrosis
- A Systematic Review of Oxidative Stress and Safety of Antioxidants in Diabetes: Focus on Islets and Their Defense
- Udayakumar Karunakaran, Keun-Gyu Park
- Diabetes Metab J. 2013;37(2):106-112. Published online April 16, 2013
- DOI: https://doi.org/10.4093/dmj.2013.37.2.106
- 5,169 View
- 69 Download
- 132 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader A growing body of evidence suggests that hyperglycemia-induced oxidative stress plays an important role in diabetic complications, especially β-cell dysfunction and failure. Under physiological conditions, reactive oxygen species serve as second messengers that facilitate signal transduction and gene expression in pancreatic β-cells. However, under pathological conditions, an imbalance in redox homeostasis leads to aberrant tissue damage and β-cell death due to a lack of antioxidant defense systems. Taking into account the vulnerability of islets to oxidative damage, induction of endogenous antioxidant enzymes or exogenous antioxidant administration has been proposed as a way to protect β-cells against diabetic insults. Here, we consider recent insights into how the redox response becomes deregulated under diabetic conditions, as well as the therapeutic benefits of antioxidants, which may provide clues for developing strategies aimed at the treatment or prevention of diabetes associated with β-cell failure.
-
Citations
Citations to this article as recorded by- Association Between Serum Ferritin and the Duration of Type 2 Diabetes Mellitus in a Tertiary Care Hospital in Chennai
Sankar Arumugam, Anbalagan Suyambulingam
Cureus.2024;[Epub] CrossRef - Pancreatic Parenchymal Atrophy and Pancreatic Fat Accumulation Measured by Multidetector Computed Tomography as a Stable Marker of Chronic Progressive Type 2 Diabetes Mellitus—A Cross Sectional Observational Study
Kshipra Devadiga, Khanak K Nandolia, Mahendra Singh, Pankaj Sharma, Udit Chauhan, Ravi Kant
Avicenna Journal of Medicine.2024;[Epub] CrossRef - Toward Ultrasound Molecular Imaging of Endothelial Dysfunction in Diabetes: Targets, Strategies, and Challenges
Jiahan Liu, Chen Wang, Shuo Qiu, Wenqi Sun, Guodong Yang, Lijun Yuan
ACS Applied Bio Materials.2024; 7(3): 1416. CrossRef - Interference of altered plasma trace elements profile with hyperhomocysteinemia and oxidative stress damage to insulin secretion dysfunction in Psammomys obesus: focus on the selenium
Asma Bouazza, Eric Fontaine, Xavier Leverve, Elhadj-Ahmed Koceir
Archives of Physiology and Biochemistry.2023; 129(2): 505. CrossRef - Vanillic acid potentiates insulin secretion and prevents pancreatic β-cells cytotoxicity under H2O2-induced oxidative stress
Chandan Muddahally Naganna, K. Yogendra Prasad, V. P. Mahendra, P. Ganesan, Ravi Kumar
Molecular Biology Reports.2023; 50(2): 1311. CrossRef - Pancreatic β-cell dysfunction in type 2 diabetes: Implications of inflammation and oxidative stress
Phiwayinkosi V Dludla, Sihle E Mabhida, Khanyisani Ziqubu, Bongani B Nkambule, Sithandiwe E Mazibuko-Mbeje, Sidney Hanser, Albert Kotze Basson, Carmen Pheiffer, Andre Pascal Kengne
World Journal of Diabetes.2023; 14(3): 130. CrossRef - Redox Balance in Type 2 Diabetes: Therapeutic Potential and the Challenge of Antioxidant-Based Therapy
Lital Argaev-Frenkel, Tovit Rosenzweig
Antioxidants.2023; 12(5): 994. CrossRef - Polygenic Variants Linked to Oxidative Stress and the Antioxidant System Are Associated with Type 2 Diabetes Risk and Interact with Lifestyle Factors
Youngjin Choi, Hyuk-Ku Kwon, Sunmin Park
Antioxidants.2023; 12(6): 1280. CrossRef - Food Anthocyanins: Malvidin and Its Glycosides as Promising Antioxidant and Anti-Inflammatory Agents with Potential Health Benefits
Anna Merecz-Sadowska, Przemysław Sitarek, Tomasz Kowalczyk, Karolina Zajdel, Mariusz Jęcek, Paweł Nowak, Radosław Zajdel
Nutrients.2023; 15(13): 3016. CrossRef - Selenium—More than Just a Fortuitous Sulfur Substitute in Redox Biology
Luisa B. Maia, Biplab K. Maiti, Isabel Moura, José J. G. Moura
Molecules.2023; 29(1): 120. CrossRef - Nitroxyl Radical as a Theranostic Contrast Agent in Magnetic Resonance Redox Imaging
Ken-ichiro Matsumoto, Ikuo Nakanishi, Zhivko Zhelev, Rumiana Bakalova, Ichio Aoki
Antioxidants & Redox Signaling.2022; 36(1-3): 95. CrossRef - Speciation study and biological activity of copper (II) complexes with picolinic and 6-methylpicolinic acid with different components of blood serum of low molecular mass in KNO3 1.0 mol·L−1 at 25 °C
Edgar Del Carpio, María L. Serrano, Lino Hernández, Waleska Madden, Vito Lubes, Vanessa R. Landaeta, Rafael E. Rodríguez-Lugo, Giuseppe Lubes, Anita Stern, Carlos Ciangherotti, Lissette Jiménez
Polyhedron.2022; 211: 115562. CrossRef - Pharmaceutical formulation and polymer chemistry for cell encapsulation applied to the creation of a lab-on-a-chip bio-microsystem
Armin Mooranian, Melissa Jones, Corina Mihaela Ionescu, Daniel Walker, Susbin Raj Wagle, Bozica Kovacevic, Jacqueline Chester, Thomas Foster, Edan Johnston, Momir Mikov, Hani Al-Salami
Therapeutic Delivery.2022; 13(1): 51. CrossRef - Racial Differences in Pain, Nutrition, and Oxidative Stress
Larissa J. Strath, Robert E. Sorge
Pain and Therapy.2022; 11(1): 37. CrossRef - Aerobic training reduces pancreatic fat content and improves β‐cell function: A randomized controlled trial using IDEAL‐IQ magnetic resonance imaging
Min Li, Qidong Zheng, Joshua D. Miller, Panpan Zuo, Xiaodan Yuan, Jitao Feng, Chao Liu, Shan Bao, Qingqing Lou
Diabetes/Metabolism Research and Reviews.2022;[Epub] CrossRef - Synthesis, Antioxidant, and Antidiabetic Activities of Ketone Derivatives of Succinimide
Bushra Waheed, Syed Muhammad Mukarram Shah, Fida Hussain, Mohammad Ijaz Khan, Anwar Zeb, Muhammad Saeed Jan, Arpita Roy
Evidence-Based Complementary and Alternative Medicine.2022; 2022: 1. CrossRef - Recent Advances and Mechanistic Insights into Antibacterial Activity, Antibiofilm Activity, and Cytotoxicity of Silver Nanoparticles
Neetu Tripathi, Manoj Kumar Goshisht
ACS Applied Bio Materials.2022; 5(4): 1391. CrossRef - Chemical speciation, antioxidant activity and molecular docking of copper(II) complexes with pyridinedicarboxylic acids and different ligands of low molecular mass
Edgar Del Carpio, María L. Serrano, Lino Hernández, Waleska Madden, Vito Lubes, Vanessa R. Landaeta, Rafael E. Rodríguez-Lugo, Giuseppe Lubes, Anita Stern, Carlos Ciangherotti, Lissette Jiménez
Physics and Chemistry of Liquids.2022; 60(6): 943. CrossRef - Inflammaging and Osteoarthritis
Francesca Motta, Elisa Barone, Antonio Sica, Carlo Selmi
Clinical Reviews in Allergy & Immunology.2022; 64(2): 222. CrossRef - Oxidative Stress in Ageing and Chronic Degenerative Pathologies: Molecular Mechanisms Involved in Counteracting Oxidative Stress and Chronic Inflammation
Thobekile S. Leyane, Sandy W. Jere, Nicolette N. Houreld
International Journal of Molecular Sciences.2022; 23(13): 7273. CrossRef - Validation of the traditional medicinal use of a Mexican endemic orchid (Prosthechea karwinskii) through UPLC-ESI-qTOF-MS/MS characterization of its bioactive compounds
Gabriela Soledad Barragán-Zarate, Luicita Lagunez-Rivera, Rodolfo Solano, Candy Carranza-Álvarez, Diego Manuel Hernández-Benavides, Gerard Vilarem
Heliyon.2022; 8(7): e09867. CrossRef - N-acetyl-L-cysteine ameliorates hepatocyte pyroptosis of dog type 1 diabetes mellitus via suppression of NLRP3/NF-κB pathway
Haihua Huo, Haitong Wu, Feiyang Ma, Xinrun Li, Jianzhao Liao, Lianmei Hu, Qingyue Han, Ying Li, Jiaqiang Pan, Hui Zhang, Zhaoxin Tang, Jianying Guo
Life Sciences.2022; 306: 120802. CrossRef - Vitamin D regulates insulin and ameliorates apoptosis and oxidative stress in pancreatic tissues of rats with streptozotocin-induced diabetes
Fatima El Zahra M. Fathi, Kadry M. Sadek, Asmaa F. Khafaga, Abdel Wahab Al senosy, Hanan A. Ghoniem, Sahar Fayez, Mohamed F. Zeweil
Environmental Science and Pollution Research.2022; 29(60): 90219. CrossRef - Hypoglycemic, Hypolipidemic and Antioxidant Potentials of Ethanolic Stem Bark Extract of Anacardium occidentale in Streptozotocin-Induced Diabetic Rats
F. A Bamisaye, R. A Ibrahim, A.O. Sulyman, A.O. Jubril, Olawale Ajuwon
Nigerian Journal of Physiological Sciences.2022; 37(1): 137. CrossRef - Protective Effects of the Bilobalide on Retinal Oxidative Stress and Inflammation in Streptozotocin-Induced Diabetic Rats
Qiang Su, Jing Dong, Donglei Zhang, Lu Yang, Rupak Roy
Applied Biochemistry and Biotechnology.2022; 194(12): 6407. CrossRef - Effects of Psychotropic Medication on Somatic Sterol Biosynthesis of Adult Mice
Marta Balog, Allison C Anderson, Marija Heffer, Zeljka Korade, Karoly Mirnics
Biomolecules.2022; 12(10): 1535. CrossRef - Myricitrin and Its Solid Lipid Nanoparticle Increase Insulin Secretion and Content of Isolated Islets from the Pancreas of Male Mice
Akram Ahangarpour, Ali Akbar Oroojan
Brazilian Journal of Pharmaceutical Sciences.2022;[Epub] CrossRef - Diabetes and plant‐derived natural products: From ethnopharmacological approaches to their potential for modern drug discovery and development
Arun K. Jugran, Sandeep Rawat, Hari P. Devkota, Indra D. Bhatt, Ranbeer S. Rawal
Phytotherapy Research.2021; 35(1): 223. CrossRef - Exploring brain insulin resistance in adults with bipolar depression using extracellular vesicles of neuronal origin
Rodrigo B. Mansur, Francheska Delgado-Peraza, Mehala Subramaniapillai, Yena Lee, Michelle Iacobucci, Flora Nasri, Nelson Rodrigues, Joshua D. Rosenblat, Elisa Brietzke, Victoria E. Cosgrove, Nicole E. Kramer, Trisha Suppes, Charles L. Raison, Andrea Fagio
Journal of Psychiatric Research.2021; 133: 82. CrossRef - Protective Effects of Iridoid Glycoside from Corni Fructus on Type 2 Diabetes with Nonalcoholic Fatty Liver in Mice
Dou Niu, Xue Chen, Ting Wang, Fuxing Wang, Qiusheng Zhang, Xiaochang Xue, Jiefang Kang, Dan Qian Chen
BioMed Research International.2021; 2021: 1. CrossRef - Microdose Lithium Protects against Pancreatic Islet Destruction and Renal Impairment in Streptozotocin-Elicited Diabetes
Jiahui Zhang, Fnu Anshul, Deepak K. Malhotra, Juan Jaume, Lance D. Dworkin, Rujun Gong
Antioxidants.2021; 10(1): 138. CrossRef - p-Terphenyls From Aspergillus sp. GZWMJZ-055: Identification, Derivation, Antioxidant and α-Glycosidase Inhibitory Activities
Yanchao Xu, Yong Wang, Dan Wu, Wenwen He, Liping Wang, Weiming Zhu
Frontiers in Microbiology.2021;[Epub] CrossRef - Updated Role of Neuropeptide Y in Nicotine-Induced Endothelial Dysfunction and Atherosclerosis
Yan-li Zheng, Wan-da Wang, Mei-mei Li, Shu Lin, Hui-li Lin
Frontiers in Cardiovascular Medicine.2021;[Epub] CrossRef - IRS-2/Akt/GSK-3β/Nrf2 Pathway Contributes to the Protective Effects of Chikusetsu Saponin IVa against Lipotoxicity
Lei Wang, Jialin Duan, Na Jia, Meiyou Liu, Shanshan Cao, Yan Weng, Wei Zhang, Jinyi Cao, Ruili Li, Jia Cui, Jingwen Wang, Silvana Hrelia
Oxidative Medicine and Cellular Longevity.2021; 2021: 1. CrossRef - In Vivo and In Vitro Assays Evaluating the Biological Activity of Taurine, Glucose and Energetic Beverages
Marcos Mateo-Fernández, Fernando Valenzuela-Gómez, Rafael Font, Mercedes Del Río-Celestino, Tania Merinas-Amo, Ángeles Alonso-Moraga
Molecules.2021; 26(8): 2198. CrossRef - Effect of propolis on glycemic control in patients with type 2 diabetes: an updated systematic review and meta-analysis of randomized controlled trials
Zahra Mosallanezhad, Cain Clark, Fatemeh Bahreini, Zahra Motamed, Abdolhamid Mosallanezhad, Seyedeh Fatemeh Hosseini, Aneseh Shaban-Khalaf, Zahra Sohrabi
Nutrition & Food Science .2021; 51(7): 1124. CrossRef - The Correlation between Selenium Dependent Glutathione Peroxidase Activity and Oxidant/Antioxidant Balance in Sera of Diabetic Patients with Nephropathy
Abdulateef Altuhafi, Muhammed Altun, Mahmoud Hussein Hadwan
Reports of Biochemistry and Molecular Biology.2021; 10(2): 164. CrossRef - Effect of alpha-lipoic acid on oxidative stress parameters: A systematic review and meta-analysis
Sanaz Rezaei Zonooz, Motahareh Hasani, Mojgan Morvaridzadeh, Ana Beatriz Pizarro, Hafez Heydari, Somaye Yosaee, Gholamreza Rezamand, Javad Heshmati
Journal of Functional Foods.2021; 87: 104774. CrossRef - The Mechanisms and Management of Age-Related Oxidative Stress in Male Hypogonadism Associated with Non-communicable Chronic Disease
Kristian Leisegang, Shubhadeep Roychoudhury, Petr Slama, Renata Finelli
Antioxidants.2021; 10(11): 1834. CrossRef - Роль системы врождённого иммунитета и окислительного стресса в развитии сахарного диабета 1-типа. Пероксиредоксин 6 как новый антидиабетический препарат
Е.Г. Новосёлова, О.В. Глушкова, М.О. Хренов, С.М. Лунин, Т.В. Новосёлова, С.Б. Парфенюк
Биохимия.2021; 86(12): 1840. CrossRef - Role of Innate Immunity and Oxidative Stress in the Development of Type 1 Diabetes Mellitus. Peroxiredoxin 6 as a New Anti-Diabetic Agent
Elena G. Novoselova, Olga V. Glushkova, Maxim O. Khrenov, Sergey M. Lunin, Tatyana V. Novoselova, Svetlana B. Parfenuyk
Biochemistry (Moscow).2021; 86(12-13): 1579. CrossRef - Participation of Hsp70 and Hsp90α Heat Shock Proteins in Stress Response in the Course of Type 1 Diabetes Mellitus
E. G. Novoselova, O. V. Glushkova, M. O. Khrenov, S. B. Parfenyuk, S. M. Lunin, T. V. Novoselova, E. E. Fesenko
Doklady Biological Sciences.2020; 493(1): 124. CrossRef - The correlation between blood oxidative stress and sialic acid content in diabetic patients with nephropathy, hypertension, and hyperlipidemia
Sedigheh Shahvali, Armita Shahesmaeili, Mojgan Sanjari, Somayyeh Karami-Mohajeri
Diabetology International.2020; 11(1): 19. CrossRef - Green synthesis of gold nanoparticles from Fritillaria cirrhosa and its anti-diabetic activity on Streptozotocin induced rats
Ying Guo, Nan Jiang, Li Zhang, Min Yin
Arabian Journal of Chemistry.2020; 13(4): 5096. CrossRef - The Role of Oxidative Stress in Physiopathology and Pharmacological Treatment with Pro- and Antioxidant Properties in Chronic Diseases
Andrés García-Sánchez, Alejandra Guillermina Miranda-Díaz, Ernesto Germán Cardona-Muñoz
Oxidative Medicine and Cellular Longevity.2020; 2020: 1. CrossRef - Pharmacological and Advanced Cell Respiration Effects, Enhanced by Toxic Human-Bile Nano-Pharmaceuticals of Probucol Cell-Targeting Formulations
Susbin Raj Wagle, Bozica Kovacevic, Daniel Walker, Corina Mihaela Ionescu, Melissa Jones, Goran Stojanovic, Sanja Kojic, Armin Mooranian, Hani Al-Salami
Pharmaceutics.2020; 12(8): 708. CrossRef - Triglyceride is independently correlated with insulin resistance and islet beta cell function: a study in population with different glucose and lipid metabolism states
Minglei Ma, Haibin Liu, Jie Yu, Shuli He, Pingping Li, Chunxiao Ma, Huabing Zhang, Lingling Xu, Fan Ping, Wei Li, Qi Sun, Yuxiu Li
Lipids in Health and Disease.2020;[Epub] CrossRef - Protective Effects of Grape Seed Proanthocyanidins on the Kidneys of Diabetic Rats through the Nrf2 Signalling Pathway
Yusong Ding, Haiyan Li, Yang Li, Dandan Liu, Liyuan Zhang, Tongling Wang, Tao Liu, Long Ma, Rocío De la Puerta
Evidence-Based Complementary and Alternative Medicine.2020; 2020: 1. CrossRef - The Role of CD36 in Type 2 Diabetes Mellitus: β-Cell Dysfunction and Beyond
Jun Sung Moon, Udayakumar Karunakaran, Elumalai Suma, Seung Min Chung, Kyu Chang Won
Diabetes & Metabolism Journal.2020; 44(2): 222. CrossRef - Roles of Autophagy in Oxidative Stress
Hyeong Rok Yun, Yong Hwa Jo, Jieun Kim, Yoonhwa Shin, Sung Soo Kim, Tae Gyu Choi
International Journal of Molecular Sciences.2020; 21(9): 3289. CrossRef - Antioxidant and prebiotic effects of a beverage composed by tropical fruits and yacon in alloxan-induced diabetic rats
Ana Paula DIONISIO, Luciano Bruno de CARVALHO-SILVA, Nara Menezes VIEIRA, Nedio Jair WURLITZER, Ana Carolina da Silva PEREIRA, Maria de Fatima BORGES, Deborah dos Santos GARRUTI, Idila dos Santos ARAÚJO
Food Science and Technology.2020; 40(1): 202. CrossRef - Pro-oxidant–antioxidant balance (PAB) as a prognostic index in assessing the cardiovascular risk factors: A narrative review
Hamideh Ghazizadeh, Maryam Saberi-Karimian, Maliheh Aghasizadeh, Reza Sahebi, Hamed Ghazavi, Hamed Khedmatgozar, Ameneh Timar, Mohadeseh Rohban, Ali Javandoost, Majid Ghayour-Mobarhan
Obesity Medicine.2020; 19: 100272. CrossRef - Rosemary Leaf Extract Inhibits Glycation, Breast Cancer Proliferation, and Diabetes Risks
Yixiao Shen, Jing Han, Xiaoyan Zheng, Binling Ai, Yang Yang, Dao Xiao, Lili Zheng, Zhanwu Sheng
Applied Sciences.2020; 10(7): 2249. CrossRef - Trigonella stellata reduced the deleterious effects of diabetes mellitus through alleviation of oxidative stress, antioxidant- and drug-metabolizing enzymes activities
Salah A. Sheweita, Sara A. ElHady, Hala M. Hammoda
Journal of Ethnopharmacology.2020; 256: 112821. CrossRef - A Shift Toward a Plant-Centered Diet From Young to Middle Adulthood and Subsequent Risk of Type 2 Diabetes and Weight Gain: The Coronary Artery Risk Development in Young Adults (CARDIA) Study
Yuni Choi, Nicole Larson, Daniel D. Gallaher, Andrew O. Odegaard, Jamal S. Rana, James M. Shikany, Lyn M. Steffen, David R. Jacobs
Diabetes Care.2020; 43(11): 2796. CrossRef - Ascorbic acid supplementation in type 2 diabetes mellitus
Lipeng Shi, Xuqin Du, Pei Guo, Lumei Huang, Peng Qi, Qianhui Gong
Medicine.2020; 99(45): e23125. CrossRef - Analysis of the Effect of Fish Bars Made of Bilih Fish (Mystacoleuseus padangensis Blkr) Flour to Reduce Oxidative Stress in a Diabetic Rat Model
Deni ELNOVRIZA, Hadi RIYADI, Rimbawan RIMBAWAN, Evy DAMAYANTHI, Adi WINARTO
Journal of Nutritional Science and Vitaminology.2020; 66(Supplement): S36. CrossRef - Antioxidant activity of crude ethanolic extract and fractions of Ziziphus mauritiana Lam. (Rhamnaceae) leaves from Burkina Faso
Estelle N.H. Youl, Cyrille A.P. Ouédraogo, Moustapha Gambo, Moussa Ouédraogo, Martin Kiendrebéogo, Aristide Traoré, Innocent Pierre Guissou
Journal of Basic and Clinical Physiology and Pharmacology.2019;[Epub] CrossRef - CD36 dependent redoxosomes promotes ceramide-mediated pancreatic β-cell failure via p66Shc activation
Udayakumar Karunakaran, Suma Elumalai, Jun Sung Moon, Kyu Chang Won
Free Radical Biology and Medicine.2019; 134: 505. CrossRef - Comparative proteomic analysis reveals drug resistance of Staphylococcus xylosus ATCC700404 under tylosin stress
Xin Liu, Jinpeng Wang, Mo Chen, Ruixiang Che, Wenya Ding, Fei Yu, Yonghui Zhou, Wenqiang Cui, Xing Xiaoxu, Bello-Onaghise God’spower, Yanhua Li
BMC Veterinary Research.2019;[Epub] CrossRef - The Potential of Bilih Fish (Mystacoleuseus padangensis Blkr) Flour as a Zinc Source to Control Blood Glucose and Impact on Oxidative Stress in a Diabetic Rat Model
Deni Elnovriza, Hadi Riyadi, Rimbawan ., Evy Damayanthi, Adi Winarto
Pakistan Journal of Nutrition.2019; 18(3): 264. CrossRef - Inflammaging and Oxidative Stress in Human Diseases: From Molecular Mechanisms to Novel Treatments
Zuo, Prather, Stetskiv, Garrison, Meade, Peace, Zhou
International Journal of Molecular Sciences.2019; 20(18): 4472. CrossRef - The variations of some salivary parameters as probable indices of the hereditary diabetes
Menicagli Roberto, Marotta Ortensio
International Journal of Preventive Medicine.2019; 10(1): 11. CrossRef - The Interrelationship between Job Stress with the Immune System and Functional Memory of Women Working in Diagnostic Laboratories
Mansoureh Sadeghi-Yarandi, Anahita Khodabakhshi-Koolaee, Mohammad Reza Falsafinejad, Neda Khaletbari
The Neuroscience Journal of Shefaye Khatam.2019; 7(2): 23. CrossRef - Effect of Cinnamon Administration on Fertility of Normal and Diabetic Male Rats
Mahmoud Al-Shawabk, Abdulrahim Al Jamal
Pakistan Journal of Nutrition.2019; 18(5): 491. CrossRef - White Sesame Seed Oil Mitigates Blood Glucose Level, Reduces Oxidative Stress, and Improves Biomarkers of Hepatic and Renal Function in Participants with Type 2 Diabetes Mellitus
Farhan Aslam, Sanaullah Iqbal, Muhammad Nasir, Aftab Ahmad Anjum
Journal of the American College of Nutrition.2019; 38(3): 235. CrossRef - Effect of combination of Gynura procumbens aqueous extract and Trigona spp. honey on fertility and libido of streptozotocin-induced hyperglycaemic male rats
Khaidatul Akmar, MahanemMat Noor
Asian Pacific Journal of Reproduction.2019; 8(2): 56. CrossRef - Serum Antioxidant Parameters are Significantly Increased in Patients with Type 2 Diabetes Mellitus after Consumption of Chinese Propolis: A Randomized Controlled Trial Based on Fasting Serum Glucose Level
Weina Gao, Lingling Pu, Jingyu Wei, Zhanxin Yao, Yawen Wang, Tala Shi, Liting Zhao, Changya Jiao, Changjiang Guo
Diabetes Therapy.2018; 9(1): 101. CrossRef - Baccharis trimera (Carqueja) Improves Metabolic and Redox Status in an Experimental Model of Type 1 Diabetes
Natália Nogueira do Nascimento Kaut, Ana Carolina Silveira Rabelo, Glaucy Rodrigues Araujo, Jason Guy Taylor, Marcelo Eustáquio Silva, Maria Lúcia Pedrosa, Miriam Martins Chaves, Joamyr Victor Rossoni Junior, Daniela Caldeira Costa
Evidence-Based Complementary and Alternative Medicine.2018; 2018: 1. CrossRef - The Potential of South African Herbal Tisanes, Rooibos and Honeybush in the Management of Type 2 Diabetes Mellitus
Olawale Ajuwon, Ademola Ayeleso, Gbenga Adefolaju
Molecules.2018; 23(12): 3207. CrossRef - Clinical variables and ethnicity may influenced by polymorphism of CAT −262C/T and MnSOD 47C/T antioxidant enzymes in Algerian type1 diabetes without complications
A. Eddaikra, H. Amroun, R. Raache, A. Galleze, N. Abdallah-Elhadj, M. Azzouz, F. Meçabih, B. Mechti, M.C. Abbadi, C. Touil-Boukoffa, N. Attal
Gene.2018; 670: 182. CrossRef - Crystal structure and functional characterization of selenocysteine-containing glutathione peroxidase 4 suggests an alternative mechanism of peroxide reduction
Astrid Borchert, Jacqueline Kalms, Sophia R. Roth, Marlena Rademacher, Andrea Schmidt, Hermann-Georg Holzhutter, Hartmut Kuhn, Patrick Scheerer
Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids.2018; 1863(9): 1095. CrossRef - The effects of green cardamom supplementation on blood glucose, lipids profile, oxidative stress, sirtuin-1 and irisin in type 2 diabetic patients: a study protocol for a randomized placebo-controlled clinical trial
Mohadeseh Aghasi, Shohreh Ghazi-Zahedi, Fariba Koohdani, Fereydoun Siassi, Ensieh Nasli-Esfahani, Ali Keshavarz, Mostafa Qorbani, Hoorieh Khoshamal, Asma Salari-Moghaddam, Gity Sotoudeh
BMC Complementary and Alternative Medicine.2018;[Epub] CrossRef - Mice pancreatic islets protection from oxidative stress induced by single-walled carbon nanotubes through naringin
A Ahangarpour, S Alboghobeish, AA Oroojan, MA Dehghani
Human & Experimental Toxicology.2018; 37(12): 1268. CrossRef - Chronic hyperglycemia mediated physiological alteration and metabolic distortion leads to organ dysfunction, infection, cancer progression and other pathophysiological consequences: An update on glucose toxicity
Biplab Giri, Sananda Dey, Tanaya Das, Mrinmoy Sarkar, Jhimli Banerjee, Sandeep Kumar Dash
Biomedicine & Pharmacotherapy.2018; 107: 306. CrossRef - Cognitive dysfunction and metabolic comorbidities in mood disorders: A repurposing opportunity for glucagon-like peptide 1 receptor agonists?
Rodrigo B. Mansur, Yena Lee, Mehala Subramaniapillai, Elisa Brietzke, Roger S. McIntyre
Neuropharmacology.2018; 136: 335. CrossRef - The protective effects of a novel synthetic β-elemene derivative on human umbilical vein endothelial cells against oxidative stress-induced injury: Involvement of antioxidation and PI3k/Akt/eNOS/NO signaling pathways
Khalil Ali Ahmad, Hong Ze, Jichao Chen, Farhan Ullah Khan, Chen Xuezhuo, Jinyi Xu, Ding Qilong
Biomedicine & Pharmacotherapy.2018; 106: 1734. CrossRef - Curcumin alleviates liver oxidative stress in type 1 diabetic rats
Zhenglu Xie, Binbin Wu, Guozhi Shen, Xiaqing Li, Qianying Wu
Molecular Medicine Reports.2017;[Epub] CrossRef - Treatment with a GLP−1R agonist over four weeks promotes weight loss-moderated changes in frontal-striatal brain structures in individuals with mood disorders
Rodrigo B. Mansur, Andre Zugman, Juhie Ahmed, Danielle S. Cha, Mehala Subramaniapillai, Yena Lee, Julie Lovshin, Jung G. Lee, Jae-Hon Lee, Vladislav Drobinin, Jason Newport, Elisa Brietzke, Eva Z. Reininghaus, Kang Sim, Maj Vinberg, Natalie Rasgon, Tomas
European Neuropsychopharmacology.2017; 27(11): 1153. CrossRef - Plasma vascular endothelial growth factor B levels are increased in patients with newly diagnosed type 2 diabetes mellitus and associated with the first phase of glucose-stimulated insulin secretion function of β-cell
J. Wu, H. Wei, H. Qu, Z. Feng, J. Long, Q. Ge, H. Deng
Journal of Endocrinological Investigation.2017; 40(11): 1219. CrossRef - Associations of Dietary Antioxidants and Risk of Type 2 Diabetes: Data from the 2007–2012 Korea National Health and Nutrition Examination Survey
Dan Quansah, Kyungho Ha, Shinyoung Jun, Seong-Ah Kim, Sangah Shin, Gyung-Ah Wie, Hyojee Joung
Molecules.2017; 22(10): 1664. CrossRef - Curcumin attenuates oxidative stress in liver in Type 1 diabetic rats
Zhenglu Xie, Xinqi Zeng, Xiaqing Li, Binbin Wu, Guozhi Shen, Qianying Wu, Changbiao Wu
Open Life Sciences.2017; 12(1): 452. CrossRef - Metabolic control and periodontal treatment decreases elevated oxidative stress in the early phases of type 1 diabetes onset
Cüneyt A. Aral, Özlem Nalbantoğlu, Bilge G. Nur, Mustafa Altunsoy, Kübra Aral
Archives of Oral Biology.2017; 82: 115. CrossRef - Evaluation and Application of a Novel Quantitative Antioxidant Activity Assay Based on Cellular Metabolomics
Jianteng Wei, Qingping Hu, Ningli Wang, Yewei Liu, Dong Pei, Duolong Di
Chromatographia.2017; 80(4): 617. CrossRef - C-X-C motif chemokine ligand 8 promotes endothelial cell homing via the Akt-signal transducer and activator of transcription pathway to accelerate healing of ischemic and hypoxic skin ulcers
Lei Shen, Peng Zhang, Shanqiang Zhang, Liping Xie, Lijie Yao, Weiya Lang, Jie Lian, Wei Qin, Meng Zhang, Liang Ji
Experimental and Therapeutic Medicine.2017; 13(6): 3021. CrossRef - STEAP4: its emerging role in metabolism and homeostasis of cellular iron and copper
Rachel T Scarl, C Martin Lawrence, Hannah M Gordon, Craig S Nunemaker
Journal of Endocrinology.2017; 234(3): R123. CrossRef - Current views on neuropeptide Y and diabetes-related atherosclerosis
Wei-wei Sun, Ping Zhu, Yan-chuan Shi, Chen-liang Zhang, Xu-feng Huang, Shi-yu Liang, Zhi-yuan Song, Shu Lin
Diabetes and Vascular Disease Research.2017; 14(4): 277. CrossRef - Teucrium polium extract reverses symptoms of streptozotocin-induced diabetes in rats via rebalancing the Pdx1 and FoxO1 expressions
Parvaneh Sadat Tabatabaie, Razieh Yazdanparast
Biomedicine & Pharmacotherapy.2017; 93: 1033. CrossRef - Morin activates the Nrf2-ARE pathway and reduces oxidative stress-induced DNA damage in pancreatic beta cells
Pachamuthu Vanitha, Sankareswaran Senthilkumar, Sireesh Dornadula, Sundaramurthy Anandhakumar, Palanisamy Rajaguru, Kunka Mohanram Ramkumar
European Journal of Pharmacology.2017; 801: 9. CrossRef - Antioxidant status and gut microbiota change in an aging mouse model as influenced by exopolysaccharide produced by Lactobacillus plantarum YW11 isolated from Tibetan kefir
Jian Zhang, Xiao Zhao, Yunyun Jiang, Wen Zhao, Ting Guo, Yongqiang Cao, Junwei Teng, Xiaona Hao, Juan Zhao, Zhennai Yang
Journal of Dairy Science.2017; 100(8): 6025. CrossRef - Metformin prevents glucotoxicity by alleviating oxidative and ER stress–induced CD36 expression in pancreatic beta cells
Jun Sung Moon, Udayakumar Karunakaran, Suma Elumalai, In-Kyu Lee, Hyoung Woo Lee, Yong-Woon Kim, Kyu Chang Won
Journal of Diabetes and its Complications.2017; 31(1): 21. CrossRef - Differential dose-dependent effects of zinc oxide nanoparticles on oxidative stress-mediated pancreatic β-cell death
Swati C Asani, Rinku D Umrani, Kishore M Paknikar
Nanomedicine.2017; 12(7): 745. CrossRef - Effects of Silver Nanoparticles on Multiple Drug-Resistant Strains of Staphylococcus aureus and Pseudomonas aeruginosa from Mastitis-Infected Goats: An Alternative Approach for Antimicrobial Therapy
Yu-Guo Yuan, Qiu-Ling Peng, Sangiliyandi Gurunathan
International Journal of Molecular Sciences.2017; 18(3): 569. CrossRef - Rac1-NADPH oxidase signaling promotes CD36 activation under glucotoxic conditions in pancreatic beta cells
Suma Elumalai, Udayakumar Karunakaran, In Kyu Lee, Jun Sung Moon, Kyu Chang Won
Redox Biology.2017; 11: 126. CrossRef - Changes in pancreatic histology, insulin secretion and oxidative status in diabetic rats following treatment with Ficus deltoidea and vitexin
Samsulrizal Nurdiana, Yong Meng Goh, Hafandi Ahmad, Sulaiman Md Dom, Nur Syimal’ain Azmi, Noor Syaffinaz Noor Mohamad Zin, Mahdi Ebrahimi
BMC Complementary and Alternative Medicine.2017;[Epub] CrossRef - Murraya paniculata (L.) (Orange Jasmine): Potential Nutraceuticals with Ameliorative Effect in Alloxan‐Induced Diabetic Rats
Cicero Diego Almino Menezes, Francisca Adilfa de Oliveira Garcia, Glauce Socorro de Barros Viana, Patricia Gonçalves Pinheiro, Cícero Francisco Bezerra Felipe, Thaís Rodrigues de Albuquerque, Alisson Cordeiro Moreira, Enaide Soares Santos, Maynara Rodrigu
Phytotherapy Research.2017; 31(11): 1747. CrossRef - Exploiting biological activities of brown seaweed Ishige okamurae Yendo for potential industrial applications: a review
K. K. Asanka Sanjeewa, Won Woo Lee, Jae-Il Kim, You-Jin Jeon
Journal of Applied Phycology.2017; 29(6): 3109. CrossRef - The thioredoxin and glutathione-dependent H2O2 consumption pathways in muscle mitochondria: Involvement in H2O2 metabolism and consequence to H2O2 efflux assays
Daniel Munro, Sheena Banh, Emianka Sotiri, Nahid Tamanna, Jason R. Treberg
Free Radical Biology and Medicine.2016; 96: 334. CrossRef - Effect of crocin extracted from saffron on pro-oxidant–anti-oxidant balance in subjects with metabolic syndrome: A randomized, placebo-controlled clinical trial
I. Nikbakht-Jam, M. Khademi, M. Nosrati, S. Eslami, M. Foroutan-Tanha, A. Sahebkar, S. Tavalaie, M. Ghayour-Mobarhan, G.A.A. Ferns, F. Hadizadeh, S.A.S. Tabassi, S.A. Mohajeri, M. Emamian
European Journal of Integrative Medicine.2016; 8(3): 307. CrossRef - Multicompartmental, multilayered probucol microcapsules for diabetes mellitus: Formulation characterization and effects on production of insulin and inflammation in a pancreatic β-cell line
Armin Mooranian, Rebecca Negrulj, Frank Arfuso, Hani Al-Salami
Artificial Cells, Nanomedicine, and Biotechnology.2016; 44(7): 1642. CrossRef - Lipid peroxidation is associated with poor control of type-2 diabetes mellitus
Sameer Hassan Fatani, Abdullatif Taha Babakr, EssamEldin Mohamed NourEldin, Abdalla A. Almarzouki
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2016; 10(2): S64. CrossRef - Increased Electron Paramagnetic Resonance Signal Correlates with Mitochondrial Dysfunction and Oxidative Stress in an Alzheimer’s disease Mouse Brain
Du Fang, Zhihua Zhang, Hang Li, Qing Yu, Justin T. Douglas, Anna Bratasz, Periannan Kuppusamy, Shirley ShiDu Yan, Hemachandra Reddy
Journal of Alzheimer's Disease.2016; 51(2): 571. CrossRef - Coffee silverskin extract improves glucose-stimulated insulin secretion and protects against streptozotocin-induced damage in pancreatic INS-1E beta cells
Beatriz Fernandez-Gomez, Sonia Ramos, Luis Goya, María Dolores Mesa, María Dolores del Castillo, María Ángeles Martín
Food Research International.2016; 89: 1015. CrossRef - Male Subfertility Induced by Heterozygous Expression of Catalytically Inactive Glutathione Peroxidase 4 Is Rescued in Vivo by Systemic Inactivation of the Alox15 Gene
Simone Hanna Brütsch, Marlena Rademacher, Sophia Regina Roth, Karin Müller, Susanne Eder, Dagmar Viertel, Christiane Franz, Hartmut Kuhn, Astrid Borchert
Journal of Biological Chemistry.2016; 291(45): 23578. CrossRef - Assessment of antioxidant activity, lipid profile, general biochemical and immune system responses of Wistar rats fed with dairy dessert containing Lactobacillus acidophilus La-5
C.S. Moura, P.C.B. Lollo, P.N. Morato, E.A. Esmerino, L.P. Margalho, V.A. Santos-Junior, P.T. Coimbra, L.P. Cappato, M.C. Silva, A.S. Garcia-Gomes, D. Granato, H.M. A. Bolini, A.S. Sant'Ana, A.G. Cruz, Jaime Amaya-Farfan
Food Research International.2016; 90: 275. CrossRef - Discovery of biomarkers for oxidative stress based on cellular metabolomics
Ningli Wang, Jianteng Wei, Yewei Liu, Dong Pei, Qingping Hu, Yu Wang, Duolong Di
Biomarkers.2016; 21(5): 449. CrossRef - Diabetic nephropathy and endothelial dysfunction: Current and future therapies, and emerging of vascular imaging for preclinical renal-kinetic study
Wilson KC Leung, L Gao, Parco M Siu, Christopher WK Lai
Life Sciences.2016; 166: 121. CrossRef - Brazilian Green Propolis Improves Antioxidant Function in Patients with Type 2 Diabetes Mellitus
Liting Zhao, Lingling Pu, Jingyu Wei, Jinghua Li, Jianquan Wu, Zhonghao Xin, Weina Gao, Changjiang Guo
International Journal of Environmental Research and Public Health.2016; 13(5): 498. CrossRef - Inhibition of Adenylyl Cyclase Type 5 Increases Longevity and Healthful Aging through Oxidative Stress Protection
Stephen F. Vatner, Ronald E. Pachon, Dorothy E. Vatner
Oxidative Medicine and Cellular Longevity.2015; 2015: 1. CrossRef - Recent Breakthroughs in the Antioxidant and Anti-Inflammatory Effects of Morella and Myrica Species
Bruno Silva, Ana Seca, Maria Barreto, Diana Pinto
International Journal of Molecular Sciences.2015; 16(8): 17160. CrossRef - Oxidative Stress Type Influences the Properties of Antioxidants Containing Polyphenols in RINm5F Beta Cells
Nathalie Auberval, Stéphanie Dal, William Bietiger, Elodie Seyfritz, Jean Peluso, Christian Muller, Minjie Zhao, Eric Marchioni, Michel Pinget, Nathalie Jeandidier, Elisa Maillard, Valérie Schini-Kerth, Séverine Sigrist
Evidence-Based Complementary and Alternative Medicine.2015; 2015: 1. CrossRef - CD36 initiated signaling mediates ceramide-induced TXNIP expression in pancreatic beta-cells
Udayakumar Karunakaran, Jun Sung Moon, Hyoung Woo Lee, Kyu Chang Won
Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.2015; 1852(11): 2414. CrossRef - Free radicals and related reactive species as mediators of tissue injury and disease: implications for Health
James P. Kehrer, Lars-Oliver Klotz
Critical Reviews in Toxicology.2015; 45(9): 765. CrossRef - Expression of Inactive Glutathione Peroxidase 4 Leads to Embryonic Lethality, and Inactivation of theAlox15Gene Does Not Rescue Such Knock-In Mice
Simone Hanna Brütsch, Chi Chiu Wang, Lu Li, Hannelore Stender, Nilgün Neziroglu, Constanze Richter, Hartmut Kuhn, Astrid Borchert
Antioxidants & Redox Signaling.2015; 22(4): 281. CrossRef - Islet β-cell failure in type 2 diabetes – Within the network of toxic lipids
Justyna Janikiewicz, Katarzyna Hanzelka, Kamil Kozinski, Katarzyna Kolczynska, Agnieszka Dobrzyn
Biochemical and Biophysical Research Communications.2015; 460(3): 491. CrossRef - Endoplasmic reticulum stress and Nrf2 repression in circulating cells of type 2 diabetic patients without the recommended glycemic goals
C. Mozzini, U. Garbin, C. Stranieri, A. Pasini, E. Solani, I. A. Tinelli, L. Cominacini, A.M. Fratta Pasini
Free Radical Research.2015; 49(3): 244. CrossRef - El estrés oxidativo como predictor de longevidad; estudio de casos y controles
Ángel Belenguer Varea, Kheira Mohamed Abdelaziz, Juan Antonio Avellana Zaragoza, Consuelo Borrás Blasco, Paula Sanchis Aguilar, José Viña Ribes
Revista Española de Geriatría y Gerontología.2015; 50(1): 16. CrossRef - Microbial phenolic metabolites improve glucose-stimulated insulin secretion and protect pancreatic beta cells against tert-butyl hydroperoxide-induced toxicity via ERKs and PKC pathways
Elisa Fernández-Millán, Sonia Ramos, Carmen Alvarez, Laura Bravo, Luis Goya, María Ángeles Martín
Food and Chemical Toxicology.2014; 66: 245. CrossRef - Decreased serum CA19‐9 is associated with improvement of insulin resistance and metabolic control in patients with obesity and type 2 diabetes after Roux‐en‐Y gastric bypass
Yinfang Tu, Haoyong Yu, Pin Zhang, Jianzhong Di, Xiaodong Han, Songhua Wu, Yuqian Bao, Weiping Jia
Journal of Diabetes Investigation.2014; 5(6): 694. CrossRef - Oxidative Stress Is Associated with an Increased Antioxidant Defense in Elderly Subjects: A Multilevel Approach
Gemma Flores-Mateo, Roberto Elosua, Teresa Rodriguez-Blanco, Josep Basora-Gallisà, Mònica Bulló, Jordi Salas-Salvadó, Miguel Ángel Martínez-González, Ramon Estruch, Dolores Corella, Montserrat Fitó, Miquel Fiol, Fernando Arós, Enrique Gómez-Gracia, Isaac
PLoS ONE.2014; 9(9): e105881. CrossRef - Inflamed moods: A review of the interactions between inflammation and mood disorders
Joshua D. Rosenblat, Danielle S. Cha, Rodrigo B. Mansur, Roger S. McIntyre
Progress in Neuro-Psychopharmacology and Biological Psychiatry.2014; 53: 23. CrossRef - Differences in pancreatic volume, fat content, and fat density measured by multidetector-row computed tomography according to the duration of diabetes
Soo Lim, Jae Hyun Bae, Eun Ju Chun, Haeryoung Kim, So Yeon Kim, Kyoung Min Kim, Sung Hee Choi, Kyong Soo Park, Jose C. Florez, Hak Chul Jang
Acta Diabetologica.2014; 51(5): 739. CrossRef - Role of Lipid Peroxidation Products, Plasma Total Antioxidant Status, and Cu-, Zn-Superoxide Dismutase Activity as Biomarkers of Oxidative Stress in Elderly Prediabetics
Sylwia Dzięgielewska-Gęsiak, Ewa Wysocka, Sławomir Michalak, Ewa Nowakowska-Zajdel, Teresa Kokot, Małgorzata Muc-Wierzgoń
Oxidative Medicine and Cellular Longevity.2014; 2014: 1. CrossRef - Inhibitors ofα-glucosidase andα-amylase fromCyperus rotundus
Hong Hanh Thi Tran, Minh Chau Nguyen, Hoang Tram Le, Thi Luyen Nguyen, Thanh Binh Pham, Van Minh Chau, Hoai Nam Nguyen, Tien Dat Nguyen
Pharmaceutical Biology.2014; 52(1): 74. CrossRef - Diabetes Mellitus and Disturbances in Brain Connectivity: A Bidirectional Relationship?
Rodrigo B. Mansur, Danielle S. Cha, Hanna O. Woldeyohannes, Joanna K. Soczynska, Andre Zugman, Elisa Brietzke, Roger S. McIntyre
NeuroMolecular Medicine.2014; 16(4): 658. CrossRef - Pathogenesis of Chronic Hyperglycemia: From Reductive Stress to Oxidative Stress
Liang-Jun Yan
Journal of Diabetes Research.2014; 2014: 1. CrossRef - Vitamin C Protects against INS832/13 ^|^beta;-Cell Death and/or Dysfunction Caused by Glucolipotoxicity or 3T3-L1 Adipocyte Coculture
Ruojun WANG, Jia LIU, Xiaoxuan GUO, Fengyi GAO, Baoping JI, Feng ZHOU
Journal of Nutritional Science and Vitaminology.2014; 60(5): 313. CrossRef - Antioxidant activities of novel small-molecule polysaccharide fractions purified from Portulaca oleracea L.
Yu-Ping Li, Li-Hua Yao, Guan-Jie Wu, Xiao-Fang Pi, Yan-Chun Gong, Ruo-Shong Ye, Chen-Xi Wang
Food Science and Biotechnology.2014; 23(6): 2045. CrossRef - Anti-diabetic properties of a non-conventional radical scavenger, as compared to pioglitazone and exendin-4, in streptozotocin-nicotinamide diabetic mice
Michela Novelli, Donatella Canistro, Manuela Martano, Niccola Funel, Andrea Sapone, Simone Melega, Matilde Masini, Vincenzo De Tata, Anna Pippa, Cecilia Vecoli, Daniela Campani, Rocco De Siena, Antonio Soleti, Moreno Paolini, Pellegrino Masiello
European Journal of Pharmacology.2014; 729: 37. CrossRef - Therapeutic Roles of Heme Oxygenase-1 in Metabolic Diseases: Curcumin and Resveratrol Analogues as Possible Inducers of Heme Oxygenase-1
Yong Son, Ju Hwan Lee, Hun-Taeg Chung, Hyun-Ock Pae
Oxidative Medicine and Cellular Longevity.2013; 2013: 1. CrossRef - Endoplasmic Reticulum Oxidoreductin-1α (Ero1α) Improves Folding and Secretion of Mutant Proinsulin and Limits Mutant Proinsulin-induced Endoplasmic Reticulum Stress
Jordan Wright, Julia Birk, Leena Haataja, Ming Liu, Thomas Ramming, Michael A. Weiss, Christian Appenzeller-Herzog, Peter Arvan
Journal of Biological Chemistry.2013; 288(43): 31010. CrossRef - Moving on from GWAS: Functional Studies on the G6PC2 Gene Implicated in the Regulation of Fasting Blood Glucose
Richard M. O’Brien
Current Diabetes Reports.2013; 13(6): 768. CrossRef
- Association Between Serum Ferritin and the Duration of Type 2 Diabetes Mellitus in a Tertiary Care Hospital in Chennai
- Transcriptional Regulation of Pyruvate Dehydrogenase Kinase
- Ji Yun Jeong, Nam Ho Jeoung, Keun-Gyu Park, In-Kyu Lee
- Diabetes Metab J. 2012;36(5):328-335. Published online October 18, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.5.328
- 5,567 View
- 122 Download
- 110 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader The pyruvate dehydrogenase complex (PDC) activity is crucial to maintains blood glucose and ATP levels, which largely depends on the phosphorylation status by pyruvate dehydrogenase kinase (PDK) isoenzymes. Although it has been reported that PDC is phosphorylated and inactivated by PDK2 and PDK4 in metabolically active tissues including liver, skeletal muscle, heart, and kidney during starvation and diabetes, the precise mechanisms by which expression of PDK2 and PDK4 are transcriptionally regulated still remains unclear. Insulin represses the expression of PDK2 and PDK4 via phosphorylation of FOXO through PI3K/Akt signaling pathway. Several nuclear hormone receptors activated due to fasting or increased fat supply, including peroxisome proliferator-activated receptors, glucocorticoid receptors, estrogen-related receptors, and thyroid hormone receptors, also participate in the up-regulation of PDK2 and PDK4; however, the endogenous ligands that bind those nuclear receptors have not been identified. It has been recently suggested that growth hormone, adiponectin, epinephrine, and rosiglitazone also control the expression of PDK4 in tissue-specific manners. In this review, we discuss several factors involved in the expressional regulation of PDK2 and PDK4, and introduce current studies aimed at providing a better understanding of the molecular mechanisms that underlie the development of metabolic diseases such as diabetes.
-
Citations
Citations to this article as recorded by- Molecules and targets of antidiabetic interest
Kavishankar Gawli, Kavya Sritha Bojja
Phytomedicine Plus.2024; 4(1): 100506. CrossRef - Transcriptome analysis reveals dysfunction of the endoplasmic reticulum protein processing in the sonic muscle of small yellow croaker (Larimichthys polyactis) following noise exposure
Xuguang Zhang, Xianming Tang, Jianan Xu, Yueping Zheng, Jun Lin, Huafeng Zou
Marine Environmental Research.2024; 194: 106299. CrossRef - Enhancing aortic valve drug delivery with PAR2-targeting magnetic nano-cargoes for calcification alleviation
Jinyong Chen, Tanchen Ren, Lan Xie, Haochang Hu, Xu Li, Miribani Maitusong, Xuhao Zhou, Wangxing Hu, Dilin Xu, Yi Qian, Si Cheng, Kaixiang Yu, Jian`an Wang, Xianbao Liu
Nature Communications.2024;[Epub] CrossRef - Natural Product-Based Glycolysis Inhibitors as a Therapeutic Strategy for Epidermal Growth Factor Receptor–Tyrosine Kinase Inhibitor-Resistant Non-Small Cell Lung Cancer
Wonyoung Park, Jung Ho Han, Shibo Wei, Eun-Sun Yang, Se-Yun Cheon, Sung-Jin Bae, Dongryeol Ryu, Hwan-Suck Chung, Ki-Tae Ha
International Journal of Molecular Sciences.2024; 25(2): 807. CrossRef - 1,5-Anhydroglucitol promotes pre-B acute lymphocytic leukemia progression by driving glycolysis and reactive oxygen species formation
Huasu Zhu, Huixian Ma, Na Dong, Min Wu, Dong Li, Linghong Liu, Qing Shi, Xiuli Ju
BMC Cancer.2023;[Epub] CrossRef - The pyruvate dehydrogenase complex: Life’s essential, vulnerable and druggable energy homeostat
Peter W. Stacpoole, Charles E. McCall
Mitochondrion.2023; 70: 59. CrossRef - A Conceptual Approach for Examining Effects of the Adolescent Bone Marrow Milieu on MSC Phenotype
Sanjana Kannikeswaran, Daniel G Whitney, Maureen J Devlin, Ying Li, Michelle S Caird, Andrea I Alford
JBMR Plus.2023;[Epub] CrossRef - Targeting PDK2 rescues stress-induced impaired brain energy metabolism
Changshui Wang, Changmeng Cui, Pengfei Xu, Li Zhu, Hongjia Xue, Beibei Chen, Pei Jiang
Molecular Psychiatry.2023; 28(10): 4138. CrossRef - Inhibition of pyruvate dehydrogenase kinase 4 ameliorates kidney ischemia-reperfusion injury by reducing succinate accumulation during ischemia and preserving mitochondrial function during reperfusion
Chang Joo Oh, Min-Ji Kim, Ji-Min Lee, Dong Hun Kim, Il-Young Kim, Sanghee Park, Yeongmin Kim, Kyung-Bok Lee, Sang-Hee Lee, Chae Won Lim, Myeongjin Kim, Jung-Yi Lee, Haushabhau S. Pagire, Suvarna H. Pagire, Myung Ae Bae, Dipanjan Chanda, Themis Thoudam, Ah
Kidney International.2023; 104(4): 724. CrossRef - High glucose promotes benign prostatic hyperplasia by downregulating PDK4 expression
Pengyu Wei, Dongxu Lin, Changcheng Luo, Mengyang Zhang, Bolang Deng, Kai Cui, Zhong Chen
Scientific Reports.2023;[Epub] CrossRef - PDK4 facilitates fibroblast functions and diabetic wound healing through regulation of HIF‐1α protein stability and gene expression
Zhouji Ma, Ran Mo, Ping Yang, Youjun Ding, Hao Zhang, Zheng Dong, Yutong Chen, Qian Tan
The FASEB Journal.2023;[Epub] CrossRef - PDK4 rescues high-glucose-induced senescent fibroblasts and promotes diabetic wound healing through enhancing glycolysis and regulating YAP and JNK pathway
Zhouji Ma, Youjun Ding, Xiaofeng Ding, Haining Mou, Ran Mo, Qian Tan
Cell Death Discovery.2023;[Epub] CrossRef - CD36 deletion ameliorates diabetic kidney disease by restoring fatty acid oxidation and improving mitochondrial function
Huimin Niu, Xiayu Ren, Enxue Tan, Xing Wan, Yu Wang, Honghong Shi, Yanjuan Hou, Lihua Wang
Renal Failure.2023;[Epub] CrossRef - PDK4 Decrease Neuronal Apoptosis via Inhibiting ROS-ASK1/P38 Pathway in Early Brain Injury After Subarachnoid Hemorrhage
Xuan Gao, Yong-Yue Gao, Hui-Ying Yan, Guang-Jie Liu, Yan Zhou, Tao Tao, Ting-Ting Yue, Cong Pang, Xiang-Xin Chen, Sen Gao, Ling-Yun Wu, Chun-Hua Hang, Wei Li
Antioxidants & Redox Signaling.2022; 36(7-9): 505. CrossRef - microRNA-15b-5p shuttled by mesenchymal stem cell-derived extracellular vesicles protects podocytes from diabetic nephropathy via downregulation of VEGF/PDK4 axis
Tiantian Zhao, Qingsong Jin, Lili Kong, Dongdong Zhang, Yaqin Teng, Liangyan Lin, Xiaoyan Yao, Yongjun Jin, Minglong Li
Journal of Bioenergetics and Biomembranes.2022; 54(1): 17. CrossRef - Water-Extracted Prunella vulgaris Alleviates Endometriosis by Reducing Aerobic Glycolysis
Min Kyoung Cho, Ling Jin, Jung Ho Han, Jung-Suk Jin, Se-Yun Cheon, Su Shin, Sung-Jin Bae, Jang-Kyung Park, Ki-Tae Ha
Frontiers in Pharmacology.2022;[Epub] CrossRef - Coenzyme A-Dependent Tricarboxylic Acid Cycle Enzymes Are Decreased in Alzheimer’s Disease Consistent With Cerebral Pantothenate Deficiency
Crystal Sang, Sasha A. Philbert, Danielle Hartland, Richard. D Unwin, Andrew W. Dowsey, Jingshu Xu, Garth J. S. Cooper
Frontiers in Aging Neuroscience.2022;[Epub] CrossRef - Identification of candidate aberrant differentially methylated/expressed genes in asthma
Zongling Wang, Lizhi Wang, Lina Dai, Yanan Wang, Erhong Li, Shuyuan An, Fengliang Wang, Dan Liu, Wen Pan
Allergy, Asthma & Clinical Immunology.2022;[Epub] CrossRef - Innervation and electrical pulse stimulation — in vitro effects on human skeletal muscle cells
Tomaz Marš, Katarina Miš, Marija Meznarič, Sonja Prpar Mihevc, Vid Jan, Fred Haugen, Boris Rogelj, Arild C. Rustan, G. Hege Thoresen, Sergej Pirkmajer, Nataša Nikolić
Applied Physiology, Nutrition, and Metabolism.2021; 46(4): 299. CrossRef - Mitochondrial Dysfunction: Cause or Consequence of Vascular Calcification?
Kanchan Phadwal, Christina Vrahnas, Ian G. Ganley, Vicky E. MacRae
Frontiers in Cell and Developmental Biology.2021;[Epub] CrossRef - BCKDK regulates the TCA cycle through PDC in the absence of PDK family during embryonic development
Lia Heinemann-Yerushalmi, Lital Bentovim, Neta Felsenthal, Ron Carmel Vinestock, Nofar Michaeli, Sharon Krief, Alon Silberman, Marina Cohen, Shifra Ben-Dor, Ori Brenner, Rebecca Haffner-Krausz, Maxim Itkin, Sergey Malitsky, Ayelet Erez, Elazar Zelzer
Developmental Cell.2021; 56(8): 1182. CrossRef - Unique adaptations in neonatal hepatic transcriptome, nutrient signaling, and one-carbon metabolism in response to feeding ethyl cellulose rumen-protected methionine during late-gestation in Holstein cows
Valentino Palombo, Abdulrahman Alharthi, Fernanda Batistel, Claudia Parys, Jessie Guyader, Erminio Trevisi, Mariasilvia D’Andrea, Juan J. Loor
BMC Genomics.2021;[Epub] CrossRef - PDK2: An Underappreciated Regulator of Liver Metabolism
Benjamin L. Woolbright, Robert A. Harris
Livers.2021; 1(2): 82. CrossRef - Endocrine Influence on Cardiac Metabolism in Development and Regeneration
Niall Graham, Guo N Huang
Endocrinology.2021;[Epub] CrossRef - Targeting Glucose Metabolism of Cancer Cells with Dichloroacetate to Radiosensitize High-Grade Gliomas
Kristina M. Cook, Han Shen, Kelly J. McKelvey, Harriet E. Gee, Eric Hau
International Journal of Molecular Sciences.2021; 22(14): 7265. CrossRef - Pyruvate dehydrogenase kinase 4‐mediated metabolic reprogramming is involved in rituximab resistance in diffuse large B‐cell lymphoma by affecting the expression of MS4A1/CD20
Duanfeng Jiang, Qiuyu Mo, Xiaoying Sun, Xiaotao Wang, Min Dong, Guozhen Zhang, Fangping Chen, Qiangqiang Zhao
Cancer Science.2021; 112(9): 3585. CrossRef - Skeletal muscle energy metabolism in obesity
Abel M. Mengeste, Arild C. Rustan, Jenny Lund
Obesity.2021; 29(10): 1582. CrossRef - Loss of prion protein control of glucose metabolism promotes neurodegeneration in model of prion diseases
Hélène Arnould, Vincent Baudouin, Anne Baudry, Luiz W. Ribeiro, Hector Ardila-Osorio, Mathéa Pietri, Cédric Caradeuc, Cynthia Soultawi, Declan Williams, Marjorie Alvarez, Carole Crozet, Fatima Djouadi, Mireille Laforge, Gildas Bertho, Odile Kellermann, Je
PLOS Pathogens.2021; 17(10): e1009991. CrossRef - Transcriptional and free radical responses to LVAD therapy
Kajari Dhar, Asmini KC, Fang Qiu, Hesham Basma, Krupa K. Savalia, Jocelyn Jones, Alexandra M. Moulton, Matthew C. Zimmerman, John Um, Daniel Anderson, Marshall Hyden, Brian D. Lowes
Translational Medicine Communications.2020;[Epub] CrossRef - Fine-tuning the metabolic rewiring and adaptation of translational machinery during an epithelial-mesenchymal transition in breast cancer cells
Tamara Fernández-Calero, Marcos Davyt, Karen Perelmuter, Cora Chalar, Giovana Bampi, Helena Persson, Juan Pablo Tosar, Völundur Hafstað, Hugo Naya, Carlos Rovira, Mariela Bollati-Fogolín, Ricardo Ehrlich, Gilles Flouriot, Zoya Ignatova, Mónica Marín
Cancer & Metabolism.2020;[Epub] CrossRef - Co-expression network analysis predicts a key role of microRNAs in the adaptation of the porcine skeletal muscle to nutrient supply
Emilio Mármol-Sánchez, Yuliaxis Ramayo-Caldas, Raquel Quintanilla, Tainã Figueiredo Cardoso, Rayner González-Prendes, Joan Tibau, Marcel Amills
Journal of Animal Science and Biotechnology.2020;[Epub] CrossRef - Stimulating pyruvate dehydrogenase complex reduces itaconate levels and enhances TCA cycle anabolic bioenergetics in acutely inflamed monocytes
Xuewei Zhu, David Long, Manal Zabalawi, Brian Ingram, Barbara K. Yoza, Peter W. Stacpoole, Charles E. McCall
Journal of Leukocyte Biology.2020; 107(3): 467. CrossRef - GPR30-Expressing Gastric Chief Cells Do Not Dedifferentiate But Are Eliminated via PDK-Dependent Cell Competition During Development of Metaplasia
Masahiro Hata, Hiroto Kinoshita, Yoku Hayakawa, Mitsuru Konishi, Mayo Tsuboi, Yukiko Oya, Ken Kurokawa, Yuki Hayata, Hayato Nakagawa, Keisuke Tateishi, Hiroaki Fujiwara, Yoshihiro Hirata, Daniel L. Worthley, Yuki Muranishi, Takahisa Furukawa, Shunsuke Kon
Gastroenterology.2020; 158(6): 1650. CrossRef - The pyruvate dehydrogenase kinase 2 (PDK2) is associated with conidiation, mycelial growth, and pathogenicity in Fusarium graminearum
Tao Gao, Dan He, Xin Liu, Fang Ji, Jianhong Xu, Jianrong Shi
Food Production, Processing and Nutrition.2020;[Epub] CrossRef - PDK2 Deficiency Prevents Ovariectomy-Induced Bone Loss in Mice by Regulating the RANKL-NFATc1 Pathway During Osteoclastogenesis
Ji-Min Lee, Min-Ji Kim, Sun Joo Lee, Byung-Gyu Kim, Je-Yong Choi, Seung Mi Lee, Hye Jin Ham, Jung-Min Koh, Jae-Han Jeon, In-Kyu Lee
Journal of Bone and Mineral Research.2020; 36(3): 553. CrossRef - Hemistepsin A suppresses colorectal cancer growth through inhibiting pyruvate dehydrogenase kinase activity
Ling Jin, Eun-Yeong Kim, Tae-Wook Chung, Chang Woo Han, So Young Park, Jung Ho Han, Sung-Jin Bae, Jong Rok Lee, Young Woo Kim, Se Bok Jang, Ki-Tae Ha
Scientific Reports.2020;[Epub] CrossRef - Neither Excessive Nitric Oxide Accumulation nor Acute Hyperglycemia Affects the N-Acetylaspartate Network in Wistar Rat Brain Cells
Marlena Zyśk, Piotr Pikul, Robert Kowalski, Krzysztof Lewandowski, Monika Sakowicz-Burkiewicz, Tadeusz Pawełczyk
International Journal of Molecular Sciences.2020; 21(22): 8541. CrossRef - PDK4 promotes vascular calcification by interfering with autophagic activity and metabolic reprogramming
Wen-Qi Ma, Xue-Jiao Sun, Yi Zhu, Nai-Feng Liu
Cell Death & Disease.2020;[Epub] CrossRef - Increased pyruvate dehydrogenase activity in skeletal muscle of growth-restricted ovine fetuses
Alexander L. Pendleton, Laurel R. Humphreys, Melissa A. Davis, Leticia E. Camacho, Miranda J. Anderson, Sean W. Limesand
American Journal of Physiology-Regulatory, Integrative and Comparative Physiology.2019; 317(4): R513. CrossRef - Geniposide Improves Glucose Homeostasis via Regulating FoxO1/PDK4 in Skeletal Muscle
Yan Li, Haiou Pan, Xuetong Zhang, Hui Wang, Shengnan Liu, Hui Zhang, Haifeng Qian, Li Wang, Hao Ying
Journal of Agricultural and Food Chemistry.2019; 67(16): 4483. CrossRef - The Effects of Sodium Dichloroacetate on Mitochondrial Dysfunction and Neuronal Death Following Hypoglycemia-Induced Injury
A Ra Kho, Bo Young Choi, Song Hee Lee, Dae Ki Hong, Jeong Hyun Jeong, Beom Seok Kang, Dong Hyeon Kang, Kyoung-Ha Park, Jae Bong Park, Sang Won Suh
Cells.2019; 8(5): 405. CrossRef - Predictive factors for the development of diabetes in cancer patients treated with phosphatidylinositol 3-kinase inhibitors
Gyuri Kim, Myungeun Yoo, Min Hee Hong, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Hye Ryun Kim, Yong-ho Lee, Byoung Chul Cho
Cancer Chemotherapy and Pharmacology.2019; 84(2): 405. CrossRef - Next generation sequencing of RNA reveals novel targets of resveratrol with possible implications for Canavan disease
Maja Dembic, Henriette S. Andersen, Jean Bastin, Thomas K. Doktor, Thomas J. Corydon, Jörn Oliver Sass, Alexandra Lopes Costa, Fatima Djouadi, Brage S. Andresen
Molecular Genetics and Metabolism.2019; 126(1): 64. CrossRef - PDK4 Augments ER–Mitochondria Contact to Dampen Skeletal Muscle Insulin Signaling During Obesity
Themis Thoudam, Chae-Myeong Ha, Jaechan Leem, Dipanjan Chanda, Jong-Seok Park, Hyo-Jeong Kim, Jae-Han Jeon, Yeon-Kyung Choi, Suthat Liangpunsakul, Yang Hoon Huh, Tae-Hwan Kwon, Keun-Gyu Park, Robert A. Harris, Kyu-Sang Park, Hyun-Woo Rhee, In-Kyu Lee
Diabetes.2019; 68(3): 571. CrossRef - Membrane-initiated cortisol action modulates early pyruvate dehydrogenase kinase 2 (pdk2) expression in fish skeletal muscle
Jorge E. Aedo, Rodrigo Zuloaga, Sebastián Boltaña, Alfredo Molina, Juan Antonio Valdés
Comparative Biochemistry and Physiology Part A: Molecular & Integrative Physiology.2019; 233: 24. CrossRef - Restoring mitochondrial biogenesis with metformin attenuates β-GP-induced phenotypic transformation of VSMCs into an osteogenic phenotype via inhibition of PDK4/oxidative stress-mediated apoptosis
Wen-Qi Ma, Xue-Jiao Sun, Ying Wang, Yi Zhu, Xi-Qiong Han, Nai-Feng Liu
Molecular and Cellular Endocrinology.2019; 479: 39. CrossRef - Changes in acetyl-CoA mediate Sik3-induced maturation of chondrocytes in endochondral bone formation
Azuma Kosai, Nanao Horike, Yoshiaki Takei, Akihiro Yamashita, Kaori Fujita, Takashi Kamatani, Noriyuki Tsumaki
Biochemical and Biophysical Research Communications.2019; 516(4): 1097. CrossRef - Enhancing cardiac glycolysis causes an increase in PDK4 content in response to short-term high-fat diet
Maria F. Newhardt, Albert Batushansky, Satoshi Matsuzaki, Zachary T. Young, Melinda West, Ngun Cer Chin, Luke I. Szweda, Michael Kinter, Kenneth M. Humphries
Journal of Biological Chemistry.2019; 294(45): 16831. CrossRef - Upregulated PDK4 expression is a sensitive marker of increased fatty acid oxidation
Ina Katrine Nitschke Pettersen, Deusdedit Tusubira, Hanan Ashrafi, Sissel Elisabeth Dyrstad, Lena Hansen, Xiao-Zheng Liu, Linn Iren Hodneland Nilsson, Nils Gunnar Løvsletten, Kjetil Berge, Hege Wergedahl, Bodil Bjørndal, Øystein Fluge, Ove Bruland, Arild
Mitochondrion.2019; 49: 97. CrossRef - Metabolic Flexibility in Cancer: Targeting the Pyruvate Dehydrogenase Kinase:Pyruvate Dehydrogenase Axis
Benjamin L. Woolbright, Ganeshkumar Rajendran, Robert A. Harris, John A. Taylor
Molecular Cancer Therapeutics.2019; 18(10): 1673. CrossRef - Clinical use of plasma lactate concentration. Part 1: Physiology, pathophysiology, and measurement
Patricia G. Rosenstein, Brett S. Tennent‐Brown, Dez Hughes
Journal of Veterinary Emergency and Critical Care.2018; 28(2): 85. CrossRef - SIRT6 deacetylase transcriptionally regulates glucose metabolism in heart
Danish Khan, Mohsen Sarikhani, Subhajit Dasgupta, Babukrishna Maniyadath, Anwit S. Pandit, Sneha Mishra, Faiz Ahamed, Abhinav Dubey, Nowrin Fathma, Hanudatta S. Atreya, Ullas Kolthur‐Seetharam, Nagalingam R. Sundaresan
Journal of Cellular Physiology.2018; 233(7): 5478. CrossRef - Metabolic Changes Associated With Muscle Expression of SOD1G93A
Gabriella Dobrowolny, Elisa Lepore, Martina Martini, Laura Barberi, Abigail Nunn, Bianca Maria Scicchitano, Antonio Musarò
Frontiers in Physiology.2018;[Epub] CrossRef - Effect of sex on glucose handling by adipocytes isolated from rat subcutaneous, mesenteric and perigonadal adipose tissue
Floriana Rotondo, Ana Cecilia Ho-Palma, Xavier Remesar, José Antonio Fernández-López, María del Mar Romero, Marià Alemany
PeerJ.2018; 6: e5440. CrossRef - Heat stress decreases metabolic flexibility in skeletal muscle of growing pigs
Lidan Zhao, Ryan P. McMillan, Guohao Xie, Samantha G. L. W. Giridhar, Lance H. Baumgard, Samer El-Kadi, Joshua Selsby, Jason Ross, Nicholas Gabler, Matthew W. Hulver, Robert P. Rhoads
American Journal of Physiology-Regulatory, Integrative and Comparative Physiology.2018; 315(6): R1096. CrossRef - Mechanisms of AMPK in the maintenance of ATP balance during energy metabolism
Rong Ke, Qicao Xu, Cong Li, Lingyu Luo, Deqiang Huang
Cell Biology International.2018; 42(4): 384. CrossRef - Advanced glycation end products accelerate calcification in VSMCs through HIF-1α/PDK4 activation and suppress glucose metabolism
Yi Zhu, Wen-Qi Ma, Xi-Qiong Han, Ying Wang, Xin Wang, Nai-Feng Liu
Scientific Reports.2018;[Epub] CrossRef - Nε-carboxymethyl-lysine promotes calcium deposition in VSMCs via intracellular oxidative stress-induced PDK4 activation and alters glucose metabolism
Wen-Qi Ma, Xi-Qiong Han, Ying Wang, Xin Wang, Yi Zhu, Nai-Feng Liu
Oncotarget.2017; 8(68): 112841. CrossRef - Pyruvate dehydrogenase kinase 4 deficiency attenuates cisplatin-induced acute kidney injury
Chang Joo Oh, Chae-Myeong Ha, Young-Keun Choi, Sungmi Park, Mi Sun Choe, Nam Ho Jeoung, Yang Hoon Huh, Hyo-Jeong Kim, Hee-Seok Kweon, Ji-min Lee, Sun Joo Lee, Jae-Han Jeon, Robert A. Harris, Keun-Gyu Park, In-Kyu Lee
Kidney International.2017; 91(4): 880. CrossRef - PPARβ/δ in human cancer
Rolf Müller
Biochimie.2017; 136: 90. CrossRef - The physiological and molecular response of Aurelia sp.1 under hypoxia
Guoshan Wang, Yu Zhen, Zhigang Yu, Yan Shi, Qing Zhao, Jianyan Wang, Tiezhu Mi
Scientific Reports.2017;[Epub] CrossRef - A Drosophila model of GDAP1 function reveals the involvement of insulin signalling in the mitochondria-dependent neuromuscular degeneration
Víctor López del Amo, Martina Palomino-Schätzlein, Marta Seco-Cervera, José Luis García-Giménez, Federico Vicente Pallardó, Antonio Pineda-Lucena, Máximo Ibo Galindo
Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.2017; 1863(3): 801. CrossRef - Western diet enhances intestinal tumorigenesis in Min/+ mice, associating with mucosal metabolic and inflammatory stress and loss of Apc heterozygosity
Mikael Niku, Anne-Maria Pajari, Laura Sarantaus, Essi Päivärinta, Markus Storvik, Anu Heiman-Lindh, Santeri Suokas, Minna Nyström, Marja Mutanen
The Journal of Nutritional Biochemistry.2017; 39: 126. CrossRef - Small heterodimer partner (SHP) deficiency protects myocardia from lipid accumulation in high fat diet-fed mice
Jung Hun Ohn, Ji Yeon Hwang, Min Kyong Moon, Hwa Young Ahn, Hwan Hee Kim, Young Do Koo, Kwang-Il Kim, Hyuk Jae Chang, Hye Seung Lee, Hak Chul Jang, Young Joo Park, Catherine Mounier
PLOS ONE.2017; 12(10): e0186021. CrossRef - Involvement of oxidative modification of proteins related to ATP synthesis in the left ventricles of hamsters with cardiomyopathy
Sahoko Ichihara, Yuka Suzuki, Jie Chang, Kentaro Kuzuya, Chisa Inoue, Yuki Kitamura, Shinji Oikawa
Scientific Reports.2017;[Epub] CrossRef - Early induction of pyruvate dehydrogenase kinase 4 by retinoic acids in adipocytes
Emilie Distel, Thomas Cadoudal, Martine Collinet, Edwards A. Park, Chantal Benelli, Sylvie Bortoli
Molecular Nutrition & Food Research.2017;[Epub] CrossRef - Oncogenic role of PDK4 in human colon cancer cells
D Leclerc, D N T Pham, N Lévesque, M Truongcao, W D Foulkes, C Sapienza, R Rozen
British Journal of Cancer.2017; 116(7): 930. CrossRef - Fasting and Glucagon Stimulate Gene Expression of Pyruvate Dehydrogenase Kinase 4 in Chickens
Kazuhisa Honda, Shoko Takagi, Kiyotaka Kurachi, Haruka Sugimoto, Takaoki Saneyasu, Hiroshi Kamisoyama
The Journal of Poultry Science.2017; 54(4): 292. CrossRef - Therapeutic Targeting of the Pyruvate Dehydrogenase Complex/Pyruvate Dehydrogenase Kinase (PDC/PDK) Axis in Cancer
Peter W Stacpoole
JNCI: Journal of the National Cancer Institute.2017;[Epub] CrossRef - Reference Gene Selection and Prednisolone Target Gene Expression in Adipose Tissues of Friesian Cattle
Sara Divari, Enrica Berio, Bartolomeo Biolatti, Francesca Tiziana Cannizzo
Journal of Agricultural and Food Chemistry.2017; 65(50): 11140. CrossRef - Histone Deacetylase Inhibitors Protect Against Pyruvate Dehydrogenase Dysfunction in Huntington's Disease
Luana Naia, Teresa Cunha-Oliveira, Joana Rodrigues, Tatiana R. Rosenstock, Ana Oliveira, Márcio Ribeiro, Catarina Carmo, Sofia I. Oliveira-Sousa, Ana I. Duarte, Michael R. Hayden, A. Cristina Rego
The Journal of Neuroscience.2017; 37(10): 2776. CrossRef - Black Adzuki Bean (Vigna angularis) Extract Protects Pancreatic β Cells and Improves Glucose Tolerance in C57BL/6J Mice Fed a High-Fat Diet
Mina Kim, Dae Keun Kim, Youn-Soo Cha
Journal of Medicinal Food.2016; 19(5): 442. CrossRef - Inflammation increases pyruvate dehydrogenase kinase 4 (PDK4) expression via the Jun N-Terminal Kinase (JNK) pathway in C2C12 cells
Hana Park, Nam Ho Jeoung
Biochemical and Biophysical Research Communications.2016; 469(4): 1049. CrossRef - Mechanisms of Vascular Calcification: The Pivotal Role of Pyruvate Dehydrogenase Kinase 4
Jaechan Leem, In-Kyu Lee
Endocrinology and Metabolism.2016; 31(1): 52. CrossRef - Molecular Mechanisms of Obesity-Induced Osteoporosis and Muscle Atrophy
Bipradas Roy, Mary E. Curtis, Letimicia S. Fears, Samuel N. Nahashon, Hugh M. Fentress
Frontiers in Physiology.2016;[Epub] CrossRef - MiR-155 Enhances Insulin Sensitivity by Coordinated Regulation of Multiple Genes in Mice
Xiaolin Lin, Yujuan Qin, Junshuang Jia, Taoyan Lin, Xia Lin, Li Chen, Hui Zeng, Yanjiang Han, Lihong Wu, Shun Huang, Meng Wang, Shenhao Huang, Raoying Xie, Liqi Liang, Yu Liu, Ruiyu Liu, Tingting Zhang, Jing Li, Shengchun Wang, Penghui Sun, Wenhua Huang,
PLOS Genetics.2016; 12(10): e1006308. CrossRef - Transforming Growth Factor β Mediates Drug Resistance by Regulating the Expression of Pyruvate Dehydrogenase Kinase 4 in Colorectal Cancer
Yang Zhang, Yi Zhang, Liying Geng, Haowei Yi, Wei Huo, Geoffrey Talmon, Yeong C. Kim, San Ming Wang, Jing Wang
Journal of Biological Chemistry.2016; 291(33): 17405. CrossRef - Metabolic Response to Heat Stress in Late-Pregnant and Early Lactation Dairy Cows: Implications to Liver-Muscle Crosstalk
Franziska Koch, Ole Lamp, Mehdi Eslamizad, Joachim Weitzel, Björn Kuhla, Andrew C. Gill
PLOS ONE.2016; 11(8): e0160912. CrossRef - Short chain acyl-CoA dehydrogenase deficiency and short-term high-fat diet perturb mitochondrial energy metabolism and transcriptional control of lipid-handling in liver
Sujoy Ghosh, Claudia Kruger, Shawna Wicks, Jacob Simon, K. Ganesh Kumar, William D. Johnson, Randall L. Mynatt, Robert C. Noland, Brenda K. Richards
Nutrition & Metabolism.2016;[Epub] CrossRef - Metabolic reprogramming by the pyruvate dehydrogenase kinase–lactic acid axis: Linking metabolism and diverse neuropathophysiologies
Mithilesh Kumar Jha, In-Kyu Lee, Kyoungho Suk
Neuroscience & Biobehavioral Reviews.2016; 68: 1. CrossRef - 1α,25-Dihydroxyvitamin D3 Regulates Mitochondrial Oxygen Consumption and Dynamics in Human Skeletal Muscle Cells
Zachary C. Ryan, Theodore A. Craig, Clifford D. Folmes, Xuewei Wang, Ian R. Lanza, Niccole S. Schaible, Jeffrey L. Salisbury, K. Sreekumaran Nair, Andre Terzic, Gary C. Sieck, Rajiv Kumar
Journal of Biological Chemistry.2016; 291(3): 1514. CrossRef - Janus and PI3-kinases mediate glucocorticoid resistance in activated chronic leukemia cells
Sina Oppermann, Avery J. Lam, Stephanie Tung, Yonghong Shi, Lindsay McCaw, Guizhei Wang, Jarkko Ylanko, Brian Leber, David Andrews, David E. Spaner
Oncotarget.2016; 7(45): 72608. CrossRef - Energy metabolic disorder is a major risk factor in severe influenza virus infection: Proposals for new therapeutic options based on animal model experiments
Hiroshi Kido, Irene L. Indalao, Hyejin Kim, Takashi Kimoto, Satoko Sakai, Etsuhisa Takahashi
Respiratory Investigation.2016; 54(5): 312. CrossRef - Fusarium graminearum pyruvate dehydrogenase kinase 1 (FgPDK1) Is Critical for Conidiation, Mycelium Growth, and Pathogenicity
Tao Gao, Jian Chen, Zhiqi Shi, Yin-Won Lee
PLOS ONE.2016; 11(6): e0158077. CrossRef - Cardiac Ryanodine Receptor (Ryr2)-mediated Calcium Signals Specifically Promote Glucose Oxidation via Pyruvate Dehydrogenase
Michael J. Bround, Rich Wambolt, Haoning Cen, Parisa Asghari, Razvan F. Albu, Jun Han, Donald McAfee, Marc Pourrier, Nichollas E. Scott, Lubos Bohunek, Jerzy E. Kulpa, S. R. Wayne Chen, David Fedida, Roger W. Brownsey, Christoph H. Borchers, Leonard J. Fo
Journal of Biological Chemistry.2016; 291(45): 23490. CrossRef - Pyruvate Dehydrogenase Kinases: Therapeutic Targets for Diabetes and Cancers
Nam Ho Jeoung
Diabetes & Metabolism Journal.2015; 39(3): 188. CrossRef - Novel molecular mechanisms involved in hormonal regulation of lactate production in Sertoli cells
Mariana Regueira, Silvana Lucía Artagaveytia, María Noel Galardo, Eliana Herminia Pellizzari, Selva Beatriz Cigorraga, Silvina Beatriz Meroni, María Fernanda Riera
REPRODUCTION.2015; 150(4): 311. CrossRef - Influence of dietary fatty acids on differentiation of human stromal vascular fraction preadipocytes
Anna Polus, Beata Kiec-Wilk, Urszula Razny, Anna Gielicz, Gerd Schmitz, Aldona Dembinska-Kiec
Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids.2015; 1851(9): 1146. CrossRef - A metabolic switch toward lipid use in glycolytic muscle is an early pathologic event in a mouse model of amyotrophic lateral sclerosis
Lavinia Palamiuc, Anna Schlagowski, Shyuan T Ngo, Aurelia Vernay, Sylvie Dirrig‐Grosch, Alexandre Henriques, Anne‐Laurence Boutillier, Joffrey Zoll, Andoni Echaniz‐Laguna, Jean‐Philippe Loeffler, Frédérique René
EMBO Molecular Medicine.2015; 7(5): 526. CrossRef - A genetic perspective on rapid evolution in cane toads (Rhinella marina)
Lee A. Rollins, Mark F. Richardson, Richard Shine
Molecular Ecology.2015; 24(9): 2264. CrossRef - Transcriptome profiling of brown adipose tissue during cold exposure reveals extensive regulation of glucose metabolism
Qin Hao, Rachita Yadav, Astrid L. Basse, Sidsel Petersen, Si B. Sonne, Simon Rasmussen, Qianhua Zhu, Zhike Lu, Jun Wang, Karine Audouze, Ramneek Gupta, Lise Madsen, Karsten Kristiansen, Jacob B. Hansen
American Journal of Physiology-Endocrinology and Metabolism.2015; 308(5): E380. CrossRef - Pyruvate Dehydrogenase Kinase 4 Promotes Vascular Calcification via SMAD1/5/8 Phosphorylation
Sun Joo Lee, Ji Yun Jeong, Chang Joo Oh, Sungmi Park, Joon-Young Kim, Han-Jong Kim, Nam Doo Kim, Young-Keun Choi, Ji-Yeon Do, Younghoon Go, Chae-Myeong Ha, Je-Yong Choi, Seung Huh, Nam Ho Jeoung, Ki-Up Lee, Hueng-Sik Choi, Yu Wang, Keun-Gyu Park, Robert A
Scientific Reports.2015;[Epub] CrossRef - Limited capacity for glucose oxidation in fetal sheep with intrauterine growth restriction
Laura D. Brown, Paul J. Rozance, Jennifer L. Bruce, Jacob E. Friedman, William W. Hay, Stephanie R. Wesolowski
American Journal of Physiology-Regulatory, Integrative and Comparative Physiology.2015; 309(8): R920. CrossRef - The long‐acting β2‐adrenoceptor agonist, indacaterol, enhances glucocorticoid receptor‐mediated transcription in human airway epithelial cells in a gene‐ and agonist‐dependent manner
T Joshi, M Johnson, R Newton, M A Giembycz
British Journal of Pharmacology.2015; 172(10): 2634. CrossRef - The Warburg effect in tumor progression: Mitochondrial oxidative metabolism as an anti-metastasis mechanism
Jianrong Lu, Ming Tan, Qingsong Cai
Cancer Letters.2015; 356(2): 156. CrossRef - The Role of Pyruvate Dehydrogenase Kinase in Diabetes and Obesity
In-Kyu Lee
Diabetes & Metabolism Journal.2014; 38(3): 181. CrossRef - Rapid in Vitro Metabolism of the Flame Retardant Triphenyl Phosphate and Effects on Cytotoxicity and mRNA Expression in Chicken Embryonic Hepatocytes
Guanyong Su, Doug Crump, Robert J. Letcher, Sean W. Kennedy
Environmental Science & Technology.2014; 48(22): 13511. CrossRef - Low force contractions induce fatigue consistent with muscle mRNA expression in people with spinal cord injury
Michael A. Petrie, Manish Suneja, Elizabeth Faidley, Richard K. Shields
Physiological Reports.2014; 2(2): e00248. CrossRef - Diisopropylamine Dichloroacetate, a Novel Pyruvate Dehydrogenase Kinase 4 Inhibitor, as a Potential Therapeutic Agent for Metabolic Disorders and Multiorgan Failure in Severe Influenza
Kazuhiko Yamane, Irene L. Indalao, Junji Chida, Yoshikazu Yamamoto, Masaaki Hanawa, Hiroshi Kido, Amy Lynn Adamson
PLoS ONE.2014; 9(5): e98032. CrossRef - Fatty Acid Transport Protein 1 (FATP1) Localizes in Mitochondria in Mouse Skeletal Muscle and Regulates Lipid and Ketone Body Disposal
Maria Guitart, Óscar Osorio-Conles, Thais Pentinat, Judith Cebrià, Judit García-Villoria, David Sala, David Sebastián, Antonio Zorzano, Antonia Ribes, Josep C. Jiménez-Chillarón, Celia García-Martínez, Anna M. Gómez-Foix, Cedric Moro
PLoS ONE.2014; 9(5): e98109. CrossRef - CRNDE, a long non-coding RNA responsive to insulin/IGF signaling, regulates genes involved in central metabolism
Blake C. Ellis, Lloyd D. Graham, Peter L. Molloy
Biochimica et Biophysica Acta (BBA) - Molecular Cell Research.2014; 1843(2): 372. CrossRef - DLK1/PREF1 regulates nutrient metabolism and protects from steatosis
Marika Charalambous, Simao Teixeira Da Rocha, Elizabeth Jane Radford, Gema Medina-Gomez, Scott Curran, Scarlett B. Pinnock, Sacri R. Ferrón, Antonio Vidal-Puig, Anne C. Ferguson-Smith
Proceedings of the National Academy of Sciences.2014; 111(45): 16088. CrossRef - The pivotal role of pyruvate dehydrogenase kinases in metabolic flexibility
Shuai Zhang, Matthew W Hulver, Ryan P McMillan, Mark A Cline, Elizabeth R Gilbert
Nutrition & Metabolism.2014;[Epub] CrossRef - Time‐dependent effects of the flame retardant tris(1,3‐dichloro‐2‐propyl) phosphate (TDCPP) on mRNA expression, in vitro and in ovo, reveal optimal sampling times for rapidly metabolized compounds
Amani Farhat, Doug Crump, Emily Porter, Suzanne Chiu, Robert J. Letcher, Guanyong Su, Sean W. Kennedy
Environmental Toxicology and Chemistry.2014; 33(12): 2842. CrossRef - Chickens from lines selected for high and low body weight show differences in fatty acid oxidation efficiency and metabolic flexibility in skeletal muscle and white adipose tissue
S Zhang, R P McMillan, M W Hulver, P B Siegel, L H Sumners, W Zhang, M A Cline, E R Gilbert
International Journal of Obesity.2014; 38(10): 1374. CrossRef - Pathway-selective Insulin Resistance and Metabolic Disease: The Importance of Nutrient Flux
Yolanda F. Otero, John M. Stafford, Owen P. McGuinness
Journal of Biological Chemistry.2014; 289(30): 20462. CrossRef - Remodeling of Oxidative Energy Metabolism by Galactose Improves Glucose Handling and Metabolic Switching in Human Skeletal Muscle Cells
Eili Tranheim Kase, Nataša Nikolić, Siril Skaret Bakke, Kaja Kamilla Bogen, Vigdis Aas, G. Hege Thoresen, Arild Christian Rustan, Darcy Johannsen
PLoS ONE.2013; 8(4): e59972. CrossRef - Association of Estrogen Receptor α GenesPvuII andXbaI Polymorphisms with Type 2 Diabetes Mellitus in the Inpatient Population of a Hospital in Southern Iran
Farzaneh Mohammadi, Mohammad Pourahmadi, Mohadeseh Mosalanejad, Houshang Jamali, Mohamed Amin Ghobadifar, Saeideh Erfanian
Diabetes & Metabolism Journal.2013; 37(4): 270. CrossRef - The orphan nuclear receptors in cancer and diabetes
Harmit S. Ranhotra
Journal of Receptors and Signal Transduction.2013; 33(4): 207. CrossRef - Genes with Aberrant Expression in Murine Preneoplastic Intestine Show Epigenetic and Expression Changes in Normal Mucosa of Colon Cancer Patients
Daniel Leclerc, Nancy Lévesque, Yuanhang Cao, Liyuan Deng, Qing Wu, Jasmine Powell, Carmen Sapienza, Rima Rozen
Cancer Prevention Research.2013; 6(11): 1171. CrossRef
- Molecules and targets of antidiabetic interest
- Relationship between Chemerin Levels and Cardiometabolic Parameters and Degree of Coronary Stenosis in Korean Patients with Coronary Artery Disease
- Yu-Jin Hah, Nam-Keong Kim, Mi-Kyung Kim, Hye-Soon Kim, Seung-Ho Hur, Hyuck-Jun Yoon, Yoon-Nyun Kim, Keun-Gyu Park
- Diabetes Metab J. 2011;35(3):248-254. Published online June 30, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.3.248
- 24,769 View
- 30 Download
- 40 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Chemerin is a novel adipokine that is associated with inflammation and adipogenesis. However, it remains unclear whether chemerin is involved in patients with cardiovascular disease. We investigated whether the serum chemerin levels of Korean patients with coronary artery disease correlated with specific cardiometabolic parameters.
Methods In total, 131 patients, all of whom had coronary artery stenosis exceeding 50%, participated in this study. Their serum chemerin levels and cardiometabolic parameters were measured. The serum chemerin levels of two groups of patients were compared; those with one stenotic vessel (
n =68) and those with multiple stenotic vessels, including left main coronary artery disease (n =63).Results Serum chemerin levels correlated positively with the degree of coronary artery stenosis and fasting glucose, triglyceride, total cholesterol, low density lipoprotein cholesterol, and high sensitive C-reactive protein levels. The group with multiple stenotic vessels, including left main disease, had higher chemerin levels than the group with one stenotic vessel (
t =-2.129,P =0.035). Multiple binary logistic regression showed chemerin was not an independent risk factor of multiple vessel disease (odds ratio, 1.018; confidence interval, 0.997 to 1.040;P =0.091).Conclusion Serum chemerin levels have a significant correlation with several cardiometabolic risk factors and the degree of coronary artery stenosis in Korean patients with coronary artery disease. However, multiple binary logistic regression showed chemerin was not an independent risk factor of multiple vessel disease. Additional investigations are necessary to fully elucidate the role of chemerin in cardiovascular disease.
-
Citations
Citations to this article as recorded by- Adipokine chemerin overexpression in trophoblasts leads to dyslipidemia in pregnant mice: implications for preeclampsia
Lunbo Tan, Zijun Ouyang, Zhilong Chen, Fen Sun, Haichun Guo, Feng Wang, Monique Mulder, Yuan Sun, Xifeng Lu, Jian V. Zhang, A. H. Jan Danser, Koen Verdonk, Xiujun Fan, Qing Yang
Lipids in Health and Disease.2023;[Epub] CrossRef - Chemerin Levels in Acute Coronary Syndrome: Systematic Review and Meta-Analysis
Abdulrahman Ismaiel, Mohammad Zeeshan Ashfaq, Daniel-Corneliu Leucuta, Mohamed Ismaiel, Dilara Ensar Ismaiel, Stefan-Lucian Popa, Dan L Dumitrascu
Laboratory Medicine.2022; 53(6): 552. CrossRef - Prognostic value of plasma adipokine chemerin in patients with coronary artery disease
Bo Wang, Wenxin Kou, Shuya Ji, Rongrong Shen, Hongwei Ji, Jianhui Zhuang, Yifan Zhao, Bo Li, Wenhui Peng, Xuejing Yu, Hailing Li, Yawei Xu
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Role of Chemerin in Cardiovascular Diseases
Mirjana T. Macvanin, Manfredi Rizzo, Jelena Radovanovic, Alper Sonmez, Francesco Paneni, Esma R. Isenovic
Biomedicines.2022; 10(11): 2970. CrossRef - Chemerin in inflammatory diseases
Xin Su, Ye Cheng, Guoming Zhang, Bin Wang
Clinica Chimica Acta.2021; 517: 41. CrossRef - Chemerin activity in selected pathological states of human body – A systematic review
Magdalena Acewicz, Irena Kasacka
Advances in Medical Sciences.2021; 66(2): 270. CrossRef - Chemerin in atherosclerosis
Jia-Xiang Sun, Chi Zhang, Zhe-Bin Cheng, Mu-Yao Tang, Yi-Zhang Liu, Jie-Feng Jiang, Xuan Xiao, Liang Huang
Clinica Chimica Acta.2021; 520: 8. CrossRef - Serum Chemerin Concentration Is Associated with Proinflammatory Status in Chronic Coronary Syndrome
Anna Szpakowicz, Malgorzata Szpakowicz, Magda Lapinska, Marlena Paniczko, Slawomir Lawicki, Andrzej Raczkowski, Marcin Kondraciuk, Emilia Sawicka, Malgorzata Chlabicz, Marcin Kozuch, Maciej Poludniewski, Slawomir Dobrzycki, Irina Kowalska, Karol Kaminski
Biomolecules.2021; 11(8): 1149. CrossRef - Novo Efeito Cardioprotetor da L-Carnitina em Camundongos Obesos Diabéticos: Regulação da Expressão de Quemerina e CMKLRI no Coração e Tecidos Adiposos
Rezvan Amiri, Mohammad Reza Tabandeh, Seyed Ahmad Hosseini
Arquivos Brasileiros de Cardiologia.2021; 117(4): 715. CrossRef - The role of adipokines in the regulation of cardiovascular function
A. V. Karpushev, V. B. Mikhailova
"Arterial’naya Gipertenziya" ("Arterial Hypertension").2020; 25(5): 448. CrossRef - The associations among RARRES2 rs17173608 gene polymorphism, serum chemerin, and non-traditional lipid profile in patients with metabolic syndrome
Marwa A. Dahpy, Marwa K. Khairallah, Nashwa Mostafa A. Azoz, Ghada M. Ezzat
Egyptian Journal of Medical Human Genetics.2020;[Epub] CrossRef - Serum chemerin as a predictor of left ventricle hypertrophy in patients with coronary artery disease
NohaHasssanin Hanboly, Yasser Sharaf, Mervat Al-Anany, Essam Saeed
Nigerian Journal of Cardiology.2019; 16(1): 25. CrossRef - Association of Circulating Chemerin With Subclinical Parameters of Atherosclerosis
Stephanie Zylla, Marcus Dörr, Henry Völzke, Ulf Schminke, Stephan B. Felix, Matthias Nauck, Nele Friedrich
Arteriosclerosis, Thrombosis, and Vascular Biology.2018; 38(7): 1656. CrossRef - Six weeks of combined aerobic and resistance exercise using outdoor exercise machines improves fitness, insulin resistance, and chemerin in the Korean elderly: A pilot randomized controlled trial
Dong-Il Kim, Dong Hoon Lee, Sunghyun Hong, Sung-won Jo, Young-shin Won, Justin Y. Jeon
Archives of Gerontology and Geriatrics.2018; 75: 59. CrossRef - Relationship between serum chemerin levels and insulin resistance index and cardio–respiratory function in non–active obese and lean men
Mehdi Abbaszadegan, Farhad Kouhi achachluie
Advances in Obesity, Weight Management & Control.2018;[Epub] CrossRef - Serum levels of chemerin, apelin, vaspin, and omentin-1 in obese type 2 diabetic Egyptian patients with coronary artery stenosis
Tarek M.K. Motawi, Soliman G. Mahdy, Maha M. El-Sawalhi, Eman N. Ali, Rania Farag A. El-Telbany
Canadian Journal of Physiology and Pharmacology.2018; 96(1): 38. CrossRef - Plasma CXCL1 levels and TRAF3IP2 variants in patients with myocardial infarction
Safoora Pordel, Mahdi Sajedi Khanian, Mohammad Hossein Karimi, Hossein Nikoo, Mehrnoosh Doroudchi
Journal of Clinical Laboratory Analysis.2018;[Epub] CrossRef - Serum Chemerin Levels are Associated with Visceral Adiposity, Independent of Waist Circumference, in Newly Diagnosed Type 2 Diabetic Subjects
Dae Young Cheon, Jun Goo Kang, Seong Jin Lee, Sung Hee Ihm, Eun Jig Lee, Moon Gi Choi, Hyung Joon Yoo, Chul Sik Kim
Yonsei Medical Journal.2017; 58(2): 319. CrossRef - The comparison of chemerin, adiponectin and lipid profile indices in obese and non-obese adolescents
Zahra Maghsoudi, Roya Kelishadi, Mohammad Javad Hosseinzadeh-Attar
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2016; 10(2): S43. CrossRef - Chemerin processing in the myocardium: A mechanism in search of a function
Michael V.G. Latronico, Gianluigi Condorelli
Journal of Molecular and Cellular Cardiology.2016; 100: 21. CrossRef - Chemerin as an independent predictor of cardiovascular event risk
Sinan İnci, Gökhan Aksan, Pınar Doğan
Therapeutic Advances in Endocrinology and Metabolism.2016; 7(2): 57. CrossRef - Chemerin level in pregnancies complicated by preeclampsia and its relation with disease severity and neonatal outcomes
Orkun Cetin, Zehra Kurdoglu, Mertihan Kurdoglu, H. Guler Sahin
Journal of Obstetrics and Gynaecology.2016; : 1. CrossRef - Chemerin in renal dysfunction and cardiovascular disease
Mario Bonomini, Assunta Pandolfi
Vascular Pharmacology.2016; 77: 28. CrossRef - High plasma chemerin is associated with renal dysfunction and predictive for cardiovascular events — Insights from phenotype and genotype characterization
Andreas Leiherer, Axel Muendlein, Elena Kinz, Alexander Vonbank, Philipp Rein, Peter Fraunberger, Cornelia Malin, Christoph H. Saely, Heinz Drexel
Vascular Pharmacology.2016; 77: 60. CrossRef - Chemerin plays a protective role by regulating human umbilical vein endothelial cell-induced nitric oxide signaling in preeclampsia
Liqiong Wang, Tianli Yang, Yiling Ding, Yan Zhong, Ling Yu, Mei Peng
Endocrine.2015; 48(1): 299. CrossRef - Evaluation of the salivary levels of visfatin, chemerin, and progranulin in periodontal inflammation
Erkan Özcan, N. Işıl Saygun, Muhittin A. Serdar, Nezahat Kurt
Clinical Oral Investigations.2015; 19(4): 921. CrossRef - Elevated serum chemerin in Chinese women with hyperandrogenic PCOS
LiQiong Wang, Yan Zhong, YiLing Ding, XiaoBo Shi, Jian Huang, FuFan Zhu
Gynecological Endocrinology.2014; 30(10): 746. CrossRef - Chemerin reduces vascular nitric oxide/cGMP signalling in rat aorta: a link to vascular dysfunction in obesity?
Karla Bianca Neves, Núbia S. Lobato, Rhéure Alves Moreira Lopes, Fernando P. Filgueira, Camila Ziliotto Zanotto, Ana Maria Oliveira, Rita C. Tostes
Clinical Science.2014; 127(2): 111. CrossRef - Chemerin levels as predictor of acute coronary events: A case–control study nested within the veterans affairs normative aging study
Konstantinos N. Aronis, Ayse Sahin-Efe, John P. Chamberland, Avron Spiro, Pantel Vokonas, Christos S. Mantzoros
Metabolism.2014; 63(6): 760. CrossRef - The predictive value of the first-trimester maternal serum chemerin level for pre-eclampsia
Qiu-Lian Xu, Min Zhu, Yan Jin, Nan Wang, Hai-Xia Xu, Li-Mei Quan, Shan-Shan Wang, Shan-Shan Li
Peptides.2014; 62: 150. CrossRef - Evaluation of Circulating Adipokines and Abdominal Obesity as Predictors of Significant Myocardial Ischemia Using Gated Single-Photon Emission Computed Tomography
Chi-Sheng Hung, Yen-Wen Wu, Jei-Yie Huang, Pei-Ying Hsu, Ming-Fong Chen, Xin-Liang Ma
PLoS ONE.2014; 9(5): e97710. CrossRef - Towards an integrative approach to understanding the role of chemerin in human health and disease
J. L. Rourke, H. J. Dranse, C. J. Sinal
Obesity Reviews.2013; 14(3): 245. CrossRef - The association between chemerin and homeostasis assessment of insulin resistance at baseline and after weight reduction via lifestyle modifications in young obese adults
Mi Kyung Lee, Sang Hui Chu, Duk Chul Lee, Ki Yong An, Ji-Hye Park, Dong Il Kim, Jiyoung Kim, Sunghyun Hong, Jee Aee Im, Ji Won Lee, Justin Y. Jeon
Clinica Chimica Acta.2013; 421: 109. CrossRef - Elevated Chemerin Levels in Pakistani Men: An Interrelation with Metabolic Syndrome Phenotypes
Syeda Sadia Fatima, Kiymet Bozaoglu, Rehana Rehman, Faiza Alam, Abdul Shakoor Memon, Pascale Chavatte-Palmer
PLoS ONE.2013; 8(2): e57113. CrossRef - Chemerin: a potential endocrine link between obesity and type 2 diabetes
Alexandra A. Roman, Sebastian D. Parlee, Christopher J. Sinal
Endocrine.2012; 42(2): 243. CrossRef - Elastase and Tryptase Govern TNFα-Mediated Production of Active Chemerin by Adipocytes
Sebastian D. Parlee, Jenna O. McNeil, Shanmugam Muruganandan, Christopher J. Sinal, Kerry B. Goralski, Charaf Benarafa
PLoS ONE.2012; 7(12): e51072. CrossRef - Potential association between coronary artery disease and the inflammatory biomarker YKL-40 in asymptomatic patients with type 2 diabetes mellitus
Hyun Min Kim, Byung-Wan Lee, Young-Mi Song, Won Jin Kim, Hyuk-Jae Chang, Dong-Hoon Choi, Hee Tae Yu, EunSeok Kang, Bong Soo Cha, Hyun Chul Lee
Cardiovascular Diabetology.2012;[Epub] CrossRef - The association of serum chemerin level with risk of coronary artery disease in Chinese adults
Qun Yan, Yifei Zhang, Jie Hong, Weiqiong Gu, Meng Dai, Juan Shi, Ying Zhai, Weiqing Wang, Xiaoying Li, Guang Ning
Endocrine.2012; 41(2): 281. CrossRef - Epidemiology of Micro- and Macrovascular Complications of Type 2 Diabetes in Korea
Jung Hee Kim, Dae Jung Kim, Hak Chul Jang, Sung Hee Choi
Diabetes & Metabolism Journal.2011; 35(6): 571. CrossRef - Chemerin: A Novel Link between Inflammation and Atherosclerosis?
Eun-Jung Rhee
Diabetes & Metabolism Journal.2011; 35(3): 216. CrossRef
- Adipokine chemerin overexpression in trophoblasts leads to dyslipidemia in pregnant mice: implications for preeclampsia

 KDA
KDA
 First
First Prev
Prev





